If you’re trying to lose weight or control your blood glucose levels, you’re likely looking for ways to cut your intake of refined sugar. Artificial sweeteners, such as saccharin, sucralose, and xylitol, are a popular replacement for refined sugar.

However, there’s always been controversy around the potential harm these sweeteners can cause in the long run. For instance, long-term consumption can make an individual more susceptible to type 2 diabetes and weight gain. That, in turn, can increase the risk of cardiovascular diseases.
A recent study by the French National Institute of Health and Medical Research substantiates that claim. The report, published in The BMJ, found a higher rate of cardiovascular disease events in participants who consumed higher levels of artificial sweeteners.
A Closer Look at the Study
The study involving more than 170,000 French citizens commenced in 2009 with participants aged 18 years and older. The average age of the participants was 42 years, and a majority of them were females.
The researchers regularly collected information about the participants’ dietary habits, including their consumption of artificial sweeteners. Nearly 37% of participants used such sweeteners and consumed 42.46 mg/day on average.
The artificial sweeteners consumed by the participants included the following:
- Aspartame
- Acesulfame potassium
- Sucralose
- Saccharin
- Steviol glycosides (and more)
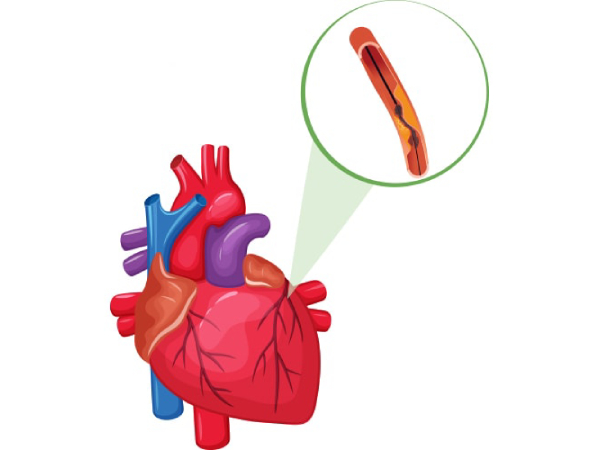
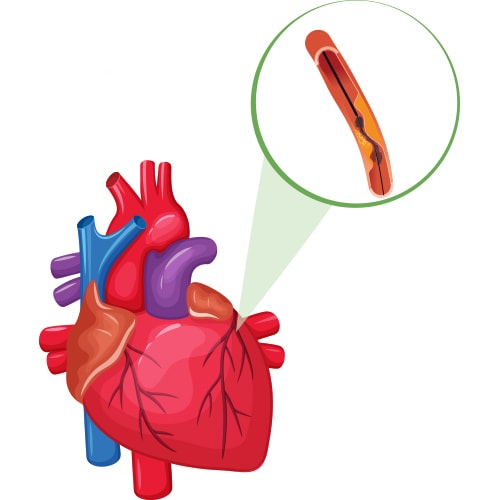
At the end of the study, the researchers uncovered a direct correlation between the intake of artificial sweeteners and the risk of heart-related ailments. Higher consumers of such sweeteners had a 9% higher incidence of cardiovascular diseases and an 18% higher incidence of cerebrovascular diseases.
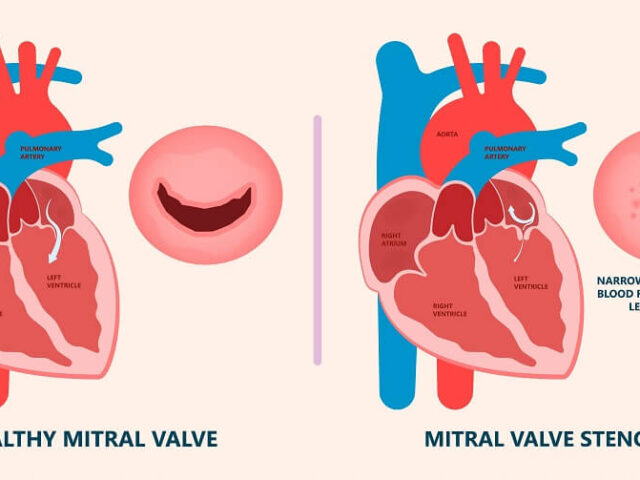
While aspartame was associated with an increased risk of strokes, acesulfame potassium and sucralose were linked with a higher risk of coronary heart disease.
What Does That Mean For You?
The recent study of French nationals echoes previous claims about the harmful effects of artificial sweeteners. Long-term consumption of these sweeteners can be detrimental to your cardiac health.
However, that doesn’t mean you should completely steer clear of them. Occasional intake within the permissible limits won’t pose any threat to you. The recommended limit depends on your body weight and the type of sweeteners.
If you’re looking to lose weight, get your blood sugar under control, or embrace healthy eating habits, your best bet is to consult a certified nutritionist. Also, it’s a good idea to consider natural alternatives to refined sugar. These include allulose and stevia.
Additionally, consider staying away from processed and packaged foods. Many of these items contain artificial sweeteners. Also, they don’t have a high nutritional value and could increase your cholesterol levels.
In Conclusion
Regular consumption of artificial sweeteners like aspartame and sucralose can have an adverse effect on your heart. They increase your risk of coronary heart disease, strokes, and other ailments.
If you’re looking for ways to minimize your refined sugar intake, consider natural alternatives like stevia. Also, consult a doctor or nutritionist to understand the side effects of different refined sugar replacements.
Dr. C Raghu is an eminent cardiologist with decades of experience. He’s helped countless patients lead healthier lives. If you or anyone you know has been diagnosed with a cardiovascular ailment, feel free to reach out to Dr. Raghu today.
Book Online Consultaion
Artificial Sweeteners and the Risk of Heart Disease – Blog