Why Should One Undergo Early Treatment for Aortic Stenosis?
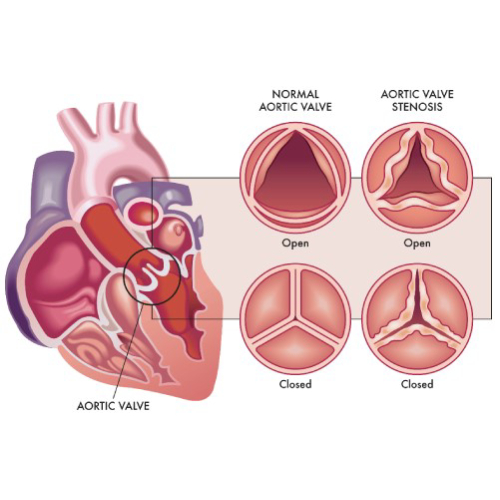
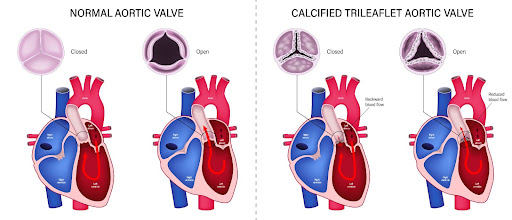
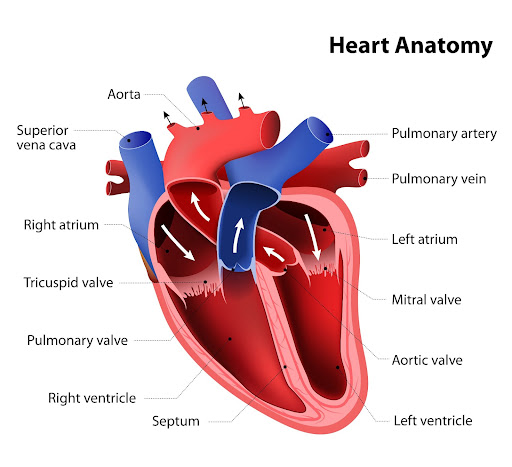
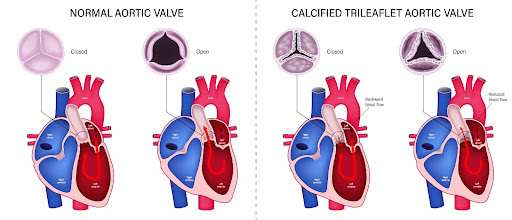
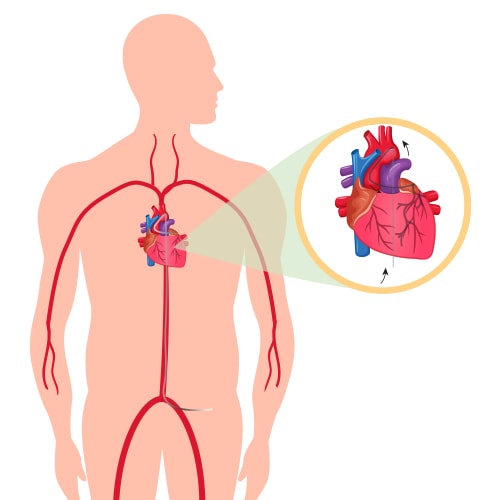
Aortic valve stenosis is a serious condition that doesn’t just affect the aortic valve. It reduces or blocks the blood supply to the aorta. That, in turn, restricts blood flow to vital organs, including the brain, kidneys, and liver.
If left untreated, aortic stenosis can lead to severe complications, including:
- Heart failure
- Blood clots and stroke
- Arrhythmias (irregular heartbeat)
- Bleeding
- Infections of the heart (including endocarditis)
All these conditions can threaten a patient’s well-being and, ultimately, result in death.
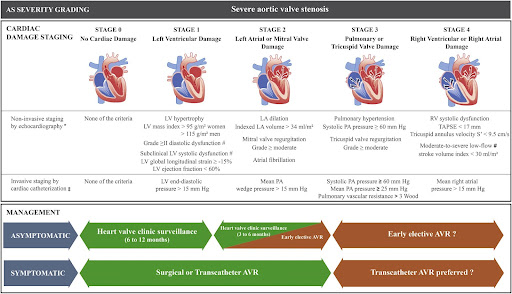
Also, it’s worth noting that aortic stenosis can worsen over time, progressing from stage A (at risk) to stage D (symptomatic severe). As the disease progresses, the prognosis becomes worse, too.
As the above graph shows, the likelihood of a patient’s survival rapidly decreases after the onset of aortic stenosis symptoms. Despite advancements in medical science, the outlook for patients with severe aortic stenosis remains poor.
That makes it crucial for aortic stenosis patients to seek treatment at the earliest. Timely diagnosis and treatment can help prevent unfavorable outcomes like arrhythmias and strokes. Also, early intervention increases the likelihood of success of treatments like aortic valve replacement and aortic valve repair.
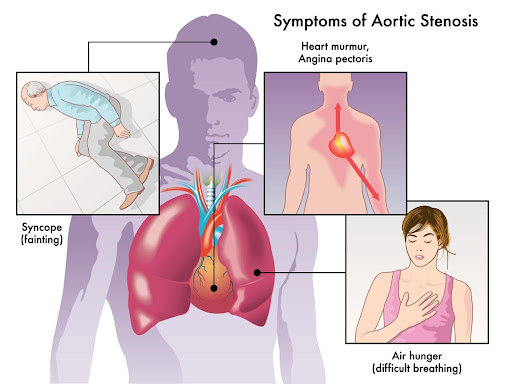
If you’re at risk of aortic stenosis due to congenital heart defects or a genetic predisposition, watch out for symptoms like heart murmur, chest pain, and shortness of breath. Also, make sure you regularly visit a cardiologist to get your heart’s chambers and valves evaluated.
What Is the Treatment for Severe Aortic Stenosis?
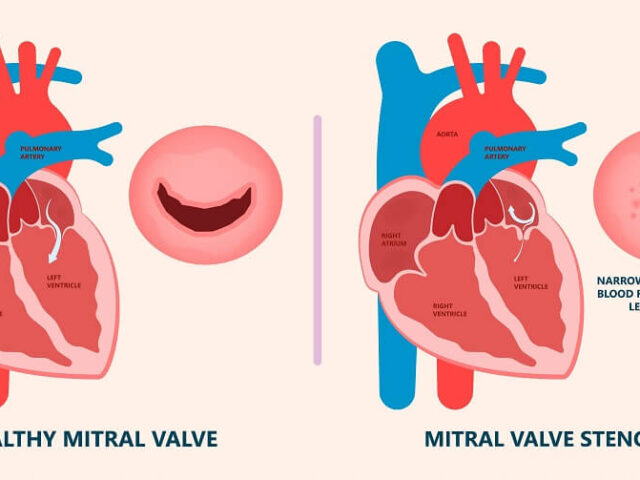
Severe aortic stenosis is characterized by significant damage to the aortic valve. Whether asymptomatic or symptomatic, the condition poses the risk of heart failure, blood clots, and even death. That makes it crucial for patients to receive treatment for aortic valve stenosis.
Patients with severe aortic stenosis need surgery to repair or replace the aortic valve. Typically, your cardiologist will recommend one of the following procedures:
Balloon Valvuloplasty
It’s a minimally invasive procedure that involves inserting a catheter with a balloon tip into an artery in the arm or groin. Once the catheter reaches the aortic valve, the balloon is inflated to expand the narrowed valve opening. Thereafter, the balloon is deflated and removed, along with the catheter.
Balloon valvuloplasty is a suitable aortic stenosis treatment option for infants and children. In adults, the aortic valve can narrow again after the procedure. However, it can be used as temporary aortic valve stenosis treatment for adults waiting for valve replacement.
Aortic Valve Replacement
It’s a type of open heart surgery where a cardiac surgeon removes the damaged aortic valve and replaces it with a mechanical valve or biological tissue valve. Biological tissue valves are made from cow, pig, or human heart tissue. They usually disintegrate over time and may need to be surgically replaced.
While mechanical valves are more durable, they increase the risk of bleeding and thromboembolic complications. Patients with mechanical valves will need to take blood thinners to minimize the risk of blood clots.
In some cases, the patient’s pulmonary valve is used to replace the aortic valve, and a mechanical valve is secured in place of the pulmonary valve. Also known as Ross Procedure, the surgery is more complex and time-consuming.
Transcatheter Aortic Valve Replacement (TAVR)

TAVR is a minimally invasive procedure suitable for patients who can’t undergo open-heart aortic valve replacement due to comorbidities or old age. In TAVR, the surgeon inserts a catheter through a tiny incision in the patient’s arm or groin. The catheter is used to transport and install a replacement valve made from cow or pig tissue to the aortic valve region. We’ll cover TAVR in more detail later in this article.
What Is Medical Treatment for Moderate Aortic Stenosis?
Mild or moderate aortic valve stenosis may not need to be treated with surgery right away. However, it’s worth noting that aortic stenosis will worsen over time, and the outlook is poor for patients in the severe stage.
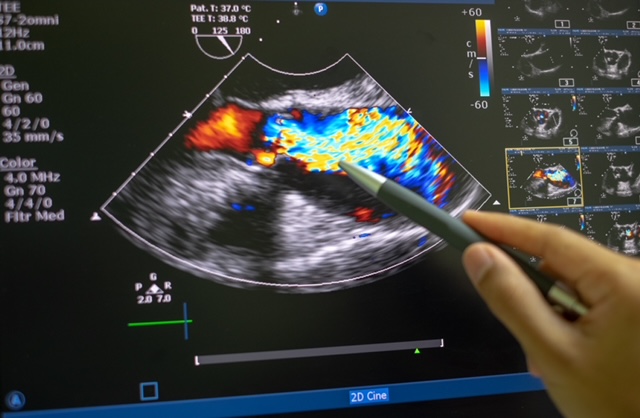
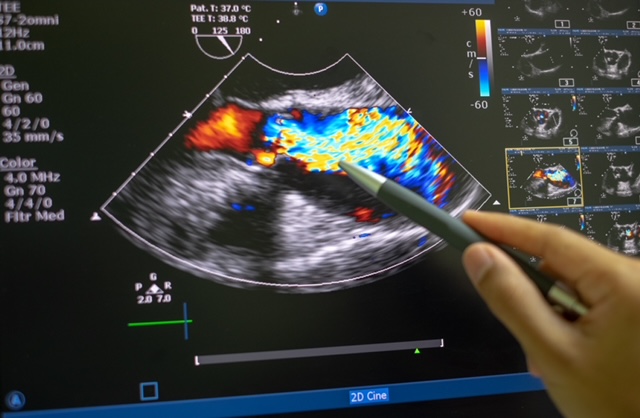
That makes it crucial for patients with moderate aortic stenosis to visit their doctor for routine evaluation and follow-ups. Your doctor might prescribe tests like echocardiogram and chest X-rays to assess the extent of valve damage.
Additionally, your doctor will recommend healthy lifestyle changes to slow down the progression of aortic stenosis. These include:
- Avoiding tobacco smoking and alcohol consumption
- Getting enough sleep
- Following a daily exercise routine
- Eating a balanced, low-fat diet
At this stage, your doctor will also focus on the management of underlying conditions, such as hypertension and chronic kidney disease, that increase the risk of aortic stenosis. They’ll prescribe suitable medications to treat these conditions.

Depending on your overall health and medical history, you can talk to your doctor and explore the possibility of undergoing aortic valve replacement (open-heart or transcatheter). Make sure you visit the doctor for regular check-ups to monitor the progression of aortic stenosis.
Surgery for Aortic Stenosis
Medical treatment and lifestyle changes can help manage the symptoms and slow down the progression of aortic valve stenosis. However, surgery is the only way to improve a patient’s longevity and quality of life.
If you’re looking for aortic stenosis treatment, you can choose from the following surgeries:
- Balloon valvuloplasty
- Aortic valve replacement (AVR)
- Transcatheter aortic valve replacement (TAVR)
Balloon valvuloplasty involves inserting a catheter with a balloon tip into an artery and inflating the balloon tip to widen the aortic valve opening. The procedure is minimally invasive and better suited for children and infants. It can also be used as a temporary fix for patients with severe aortic stenosis awaiting valve replacement.
Aortic valve replacement involves replacing the damaged aortic valve with a mechanical or biological tissue valve during open-heart surgery. If a patient has several comorbidities, they may not be an ideal candidate for AVR. In such cases, they can opt for a less invasive procedure called transcatheter aortic valve replacement.
Just like balloon valvuloplasty, TAVR also involves inserting a catheter with a balloon tip into a blood vessel. The catheter is guided to the aortic valve region and used to transport the replacement valve.
The type of surgery you’ll need depends on your current health, medical history, and the severity of aortic stenosis. It’s wiser to talk to your doctor to explore your options and choose the right surgery.
TAVR for Aortic Stenosis
Transcatheter aortic valve replacement (TAVR) is a minimally invasive procedure used for the treatment of aortic stenosis. It’s an alternative to traditional aortic valve replacement, which requires open-heart surgery.
The minimally invasive nature of TAVR makes it suitable for aortic stenosis patients who can’t undergo open-heart surgery due to comorbidities, such as lung and kidney diseases. Also known as transcatheter aortic valve implantation (TAVI), the procedure can relieve symptoms like chest pain and shortness of breath and improve a patient’s quality of life.
Unlike open-heart surgery, TAVR doesn’t require the surgeon to make a long incision on the patient’s chest. Instead, they insert a thin tube (catheter) into the patient’s artery through a tiny incision in the arm or groin area. The catheter is fitted with a balloon tip and guided to the aortic valve region.
Once the catheter reaches the aortic valve, a replacement valve (made from cow or pig tissue) is passed through it. The balloon tip inflates to securely place the replacement valve in the correct position (in place of the aortic valve). After the successful implantation of the replacement valve, the catheter and balloon tip are withdrawn.
You might receive sedatives before the procedure to help you relax. Also, you’ll likely have to spend the night in the ICU after undergoing TAVR. It helps your treatment team monitor your vitals and manage any complications that might arise after the procedure.
While TAVR is a fairly safe procedure, it comes with the following risks:
- Heart attack
- Stroke
- Bleeding
- Infection
- Arrhythmias
Most patients have to take anticoagulant medications to prevent the formation of blood clots. Also, your doctor might prescribe antibiotics to protect the replacement valve from infection. It’s wiser to talk to your doctor and assess the benefits and risks of TAVR before undergoing the procedure.
Book Online Consultaion
Treatment of Aortic Stenosis – Blog