In our previous blogs, we’ve discussed the common symptoms and treatment options for heart failure. However, the plan of treatment depends on the side of the heart that’s affected.
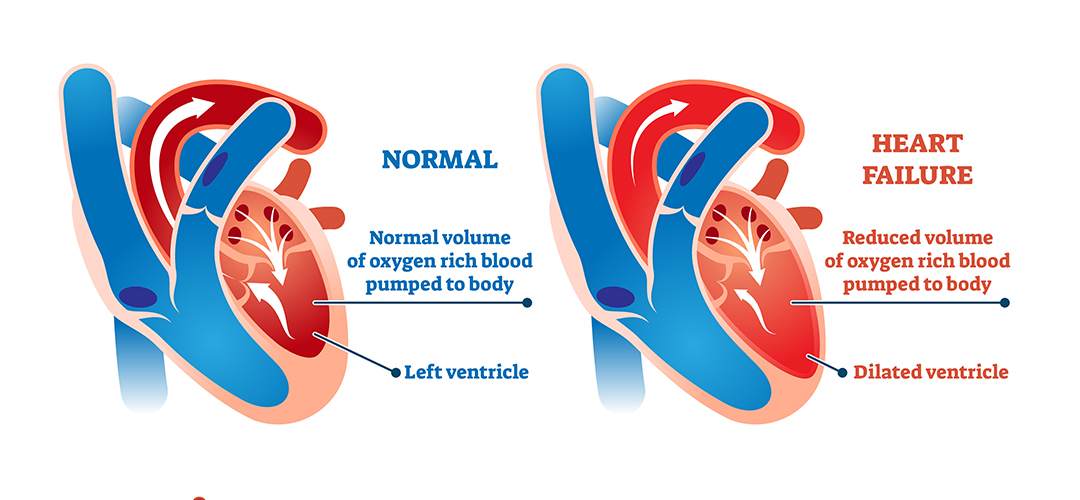
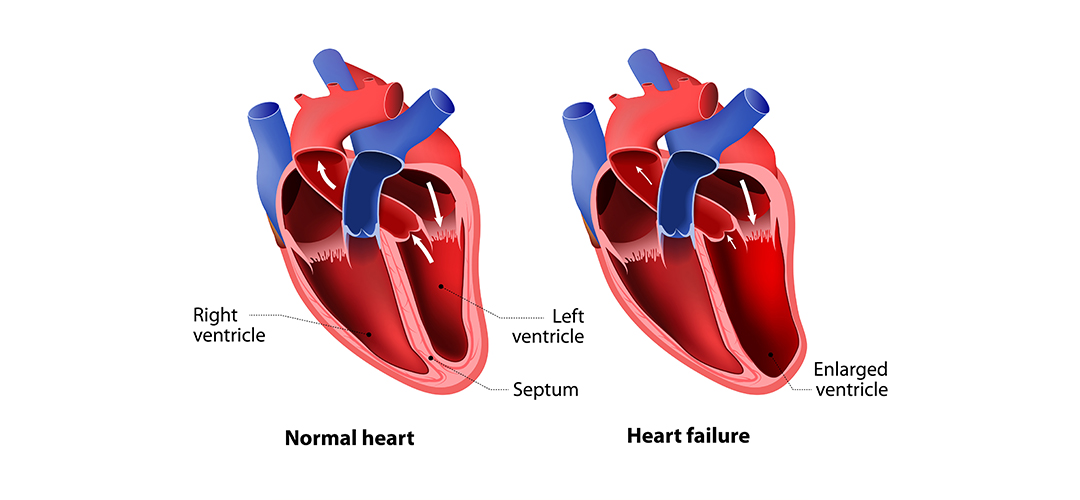
Heart failure is usually of two types – left-sided and right-sided. While left sided heart failure is the result of the weakening of the left ventricle, right sided heart failure is caused due to a weak right ventricle.

In this article, we’ll take a closer look at right sided heart failure to understand its causes and symptoms. Let’s get started.
What Is Right Sided Heart Failure?
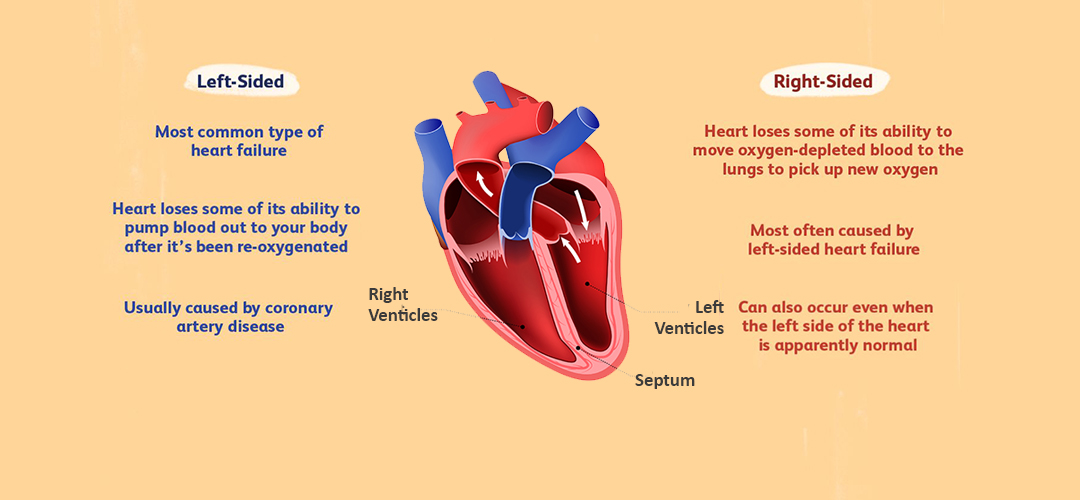
Right-sided heart failure is a condition characterized by the weakening of the heart’s right ventricle. That means the right ventricle can’t pump deoxygenated blood into the lungs with maximum efficiency. It results in a buildup of blood in the veins, thus causing swelling in the legs and abdomen.
What Causes Right-Sided Heart Failure?
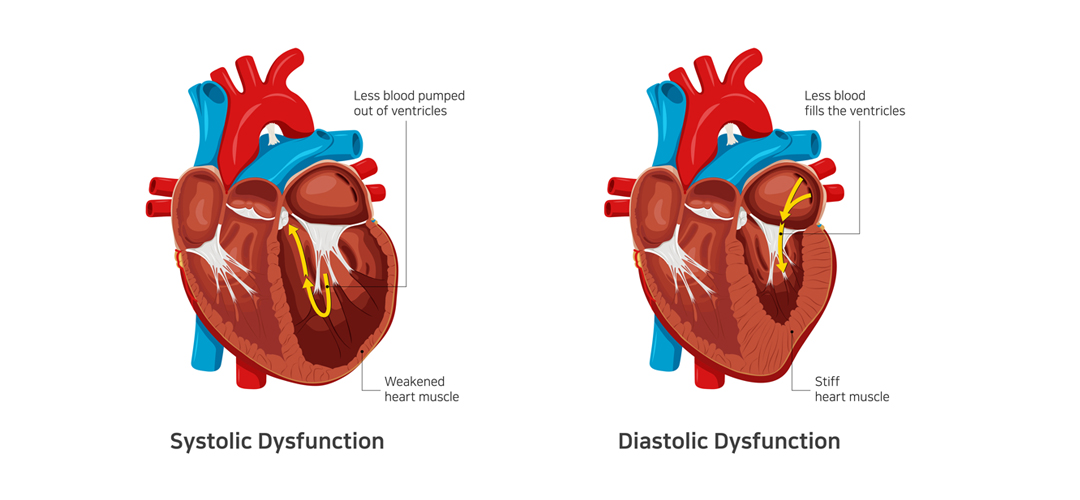
The most likely cause of right sided heart failure is a weak left ventricle. In other words, left sided heart failure eventually leads to right sided heart failure.
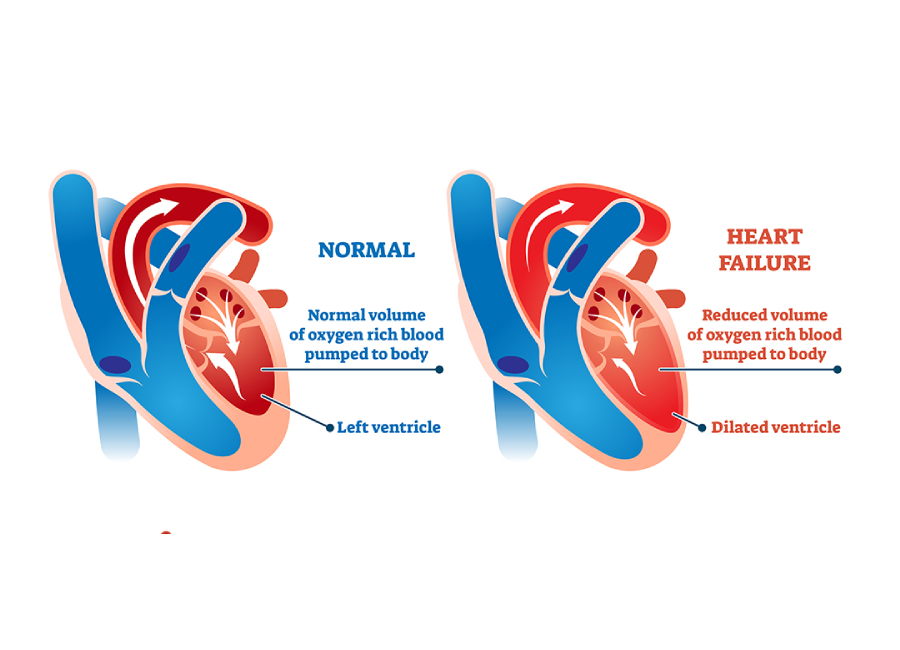
When the left ventricle becomes weak, it can’t pump an adequate amount of oxygen-rich blood into the body. It causes blood to back up into the lungs. That, in turn, means the right ventricle has to work harder to pump oxygen-depleted blood into the lungs. It results in the gradual weakening of the muscles and leads to right sided heart failure. Left sided heart failure is usually caused by coronary artery disease, hypertension, or a previous heart attack.
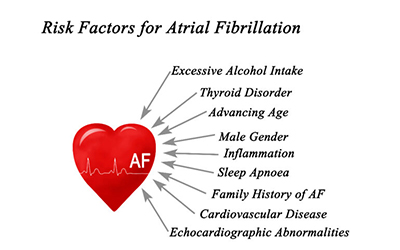
Additionally, any condition that taxes the right ventricle’s pumping power can lead to right sided heart failure. These include:
- Chronic respiratory disease
- Pulmonary hypertension
- Pulmonary embolism
What Are the Symptoms of Right Sided Heart Failure?
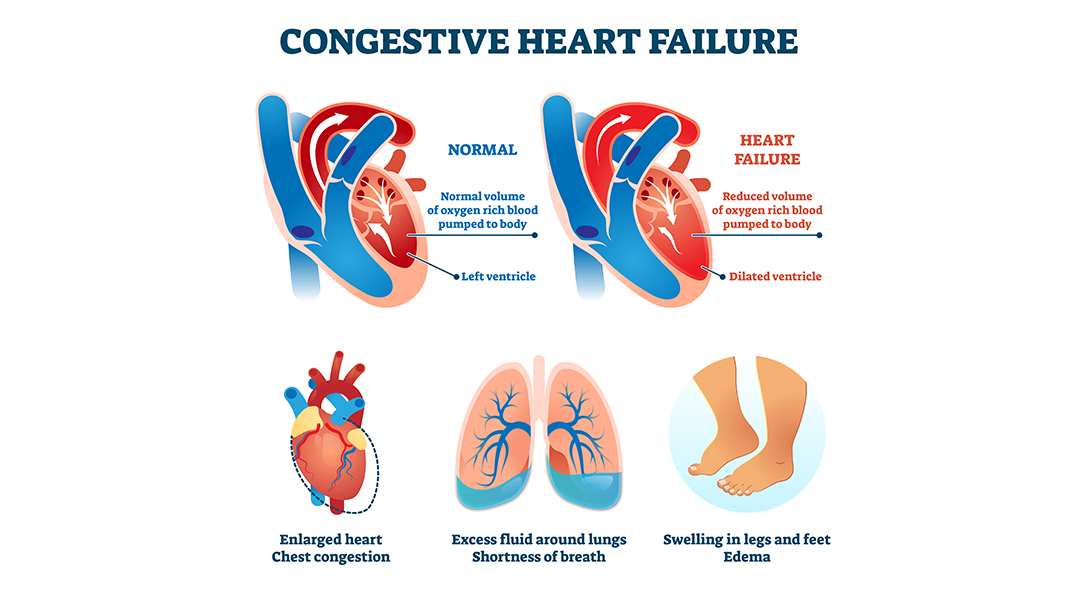
One of the most common right sided heart failure symptoms is swelling in the legs and abdomen due to fluid buildup. Accumulation of fluid in the abdomen can also cause nausea, bloating, and loss of appetite.
Other symptoms of right sided heart failure include:
- Shortness of breath
- Chest pain
- Heart palpitations
How Is Right Sided Heart Failure Diagnosed?
Firstly, a cardiologist will ask you about your symptoms and medical history. Also, they’ll perform a physical examination to check your blood pressure and heart rate. They might even use a stethoscope to identify abnormal heart sounds.
They can also recommend routine blood tests, such as complete blood count, lipid panel, and electrolyte tests. Additionally, they can order a brain natriuretic peptide test.
Besides blood tests, doctors also order the following lab tests to diagnose right sided heart failure:
- Chest X-ray
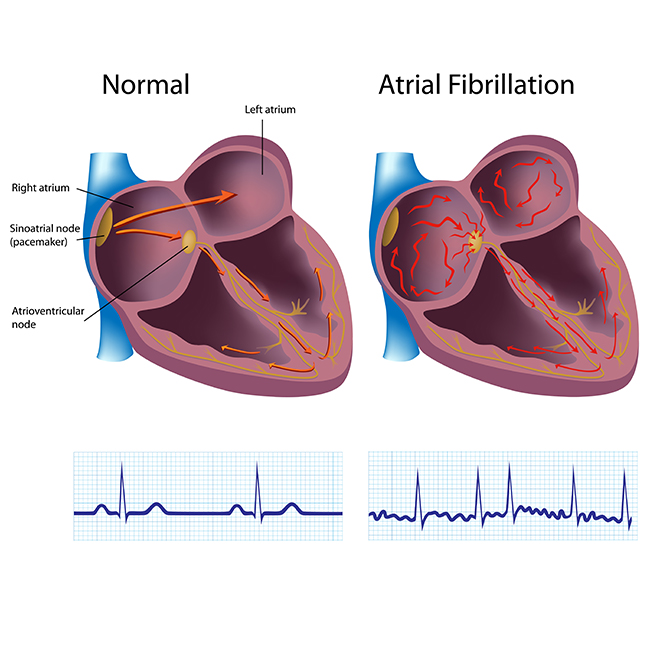
- Electrocardiogram
- Echocardiogram
- Exercise testing
- Coronary angiography
Right Sided Heart Failure vs. Congestive Heart Failure
Congestive heart failure is an outdated term that was used to refer to fluid buildup in the lungs due to a weak left ventricle. However, a more inclusive term – heart failure – is used now. Right sided heart failure is a specific type of heart failure caused by a weak right ventricle.
Final Thoughts
The most common right sided heart failure symptoms include swelling in the legs and abdomen, breathlessness, and chest pain. Doctors use a variety of tests, including ECG, coronary angiography, and chest X-ray, to diagnose the condition and determine the right course of treatment.
Dr. C Raghu is an eminent cardiologist specializing in interventional cardiology. He’s helped several patients with serious heart conditions. If you or someone you know is experiencing symptoms of heart failure, reach out to Dr. Raghu today.
Book Online Consultaion
What Is the Most Common Cause of Right-Sided Heart Failure ? – Blog