Percutaneous Interventions For Coronary Bifurcate Lesions
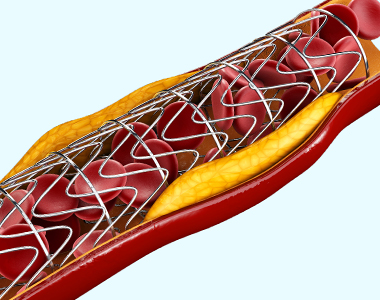
 Coronary arteries are the vessels which supply blood (oxygen and nutrients) to the heart. With age, cholesterol and fats (called plaques) are deposited on the inner walls of the arteries (atherosclerosis), thereby narrowing the lumen of the arteries.
Coronary arteries are the vessels which supply blood (oxygen and nutrients) to the heart. With age, cholesterol and fats (called plaques) are deposited on the inner walls of the arteries (atherosclerosis), thereby narrowing the lumen of the arteries.- The deposition of plaque is more likely at the site where the main coronary artery branches (bifurcation) due to the forces associated with the changes in blood flow. Narrowing (or stenoses) of the main coronary artery and the adjoining side-branch vessel is called bifurcation lesion or bifurcation blockage.
- Treating bifurcation lesions is more challenging than treating the blockage of the blood vessels that do not involve branches, as there are no stents with “Y” configuration available. Percutaneous coronary intervention is the current treatment option recommended for bifurcation lesions.
- Percutaneous coronary intervention (PCI) is a minimally invasive, non-surgical procedure that involves placing a stent (a small metal mesh) using a catheter (a thin, flexible tube) to treat the blockages in the arteries. For bifurcation blockages, two stents may be placed simultaneously.

What are the complications of PCI procedure for bifurcation lesions?
The complications associated with PCI procedures for bifurcation lesions include:
- Low success rate
- Complete obstruction of the artery caused by the formation of thrombus in the first month after implantation (subacute stent thrombosis)
- Recurrence of the blockage or the narrowing of the blood vessels (restenosis)
- Periprocedural myocardial infarction
- Stent deformation
- A gap between the stent and the arterial wall, which is greater than the stent thickness (mal-apposition)
What are the different types of PCI techniques performed for bifurcation lesions?
The following are the different types of PCI techniques used for bifurcate lesions. These techniques may vary in different cases.
T stenting technique: This technique involves positioning two stents in a ‘T’ shape. In this technique, the first stent is placed in the side branch close to the ostium (opening of the side branch), while the main branch is inflated with a balloon at low pressure. Then the second stent is placed in the main vessel.
Reverse T-stenting: This is a modified method of the classical T stenting technique. In this method, the first stent is placed in the main vessel crossing the side branch, and the second stent is placed in the side branch.
*Note: T-stenting and reverse T-stenting techniques are considered when the angle between the side branch and the main vessel is >70 degrees.
Culotte technique: In this method, the first stent is deployed into the vessel with the sharpest angulation, which covers both the main vessel and the side branch. Then, a second stent is passed through the struts of the first stent and is positioned in the main vessel only. This technique allows complete coverage of the lesion and has low rates of in-stent restenosis and periprocedural myocardial infarction.
Crush technique: In this technique, the two stents are passed at the same time in both the vessels; the stent in the main vessel more proximal than the stent in the side branch. First, the side-branch stent is paced, ad its wire and balloon are removed. Then, the main vessel stent is positioned, which flattens the protruding part of the side branch stent.
Simultaneous kissing technique: In this method, the two stents are advanced into the side branch and the main vessel and the stents are simultaneously positioned. This positioning of the two stents creates a new carina (the inflection point where the side branch separates from the main branch) in the proximal portion of the main vessel. This technique is considered only when the proximal vessel can accommodate both stents.