A heart attack, medically known as a myocardial infarction, is a severe medical emergency that can cause lasting damage to the heart muscle and even lead to death. As a leading cause of death worldwide, it shouldn't be taken lightly.
atherosclerosis / Dr Raghu
A heart attack, medically known as a myocardial infarction, is a severe medical emergency that can cause lasting damage to the heart muscle and even lead to death. As a leading cause of death worldwide, it shouldn't be taken lightly.
Heart disease is a leading cause of death worldwide. Various factors, such as stress, underlying medical conditions, and a sedentary lifestyle, make an individual more vulnerable to heart disease.
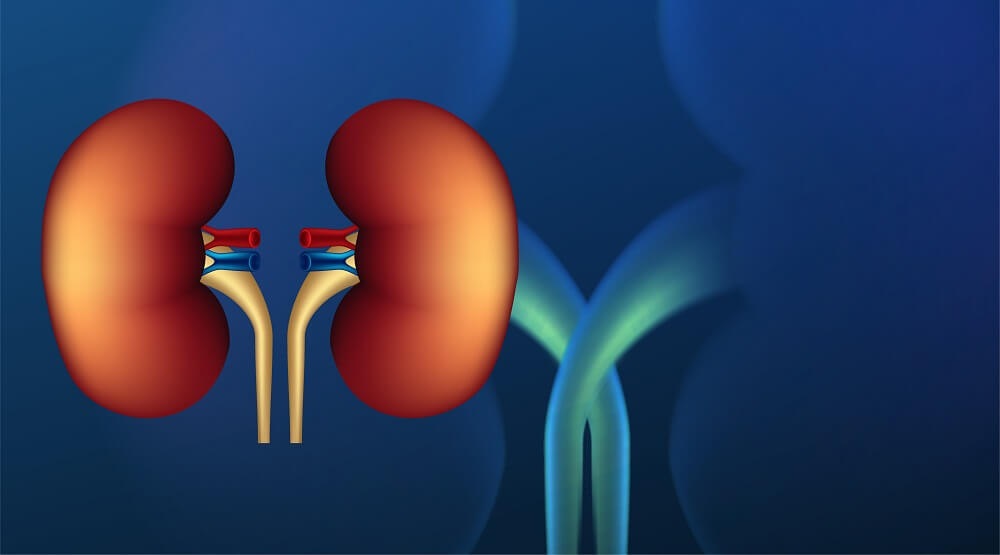
Renal artery stenosis is a serious condition that can cause life-threatening complications if left untreated. It’s characterized by the narrowing of the renal arteries that carry oxygenated blood to the kidney.
Heart failure is a condition in which the heart can’t pump enough blood to meet the body’s needs. It’s a serious condition that requires treatment by your doctor, but there are several options available. If you’re concerned about heart failure and want to know more about your options for treatment, keep reading.

What Is Heart Failure?
Heart failure occurs when your heart doesn’t pump blood as well as it should due to one or more problems with its cardiac function. The heart can’t pump blood as well because it has to work harder than normal just in order to keep up with the body’s needs for oxygen and nutrients. The extra effort causes structural changes in the heart over time.
Types of Heart Failure
Although there are many specific types of heart failure, the two broad categories are as follows:
- Heart failure with preserved ejection fraction or diastolic heart failure
- Heart failure with reduced ejection fraction or systolic heart failure
Heart failure can also be categorized depending on the side of the heart that’s affected. These include:
- Left-sided heart failure
- Right-sided heart failure
The treatment of heart failure depends on the type of heart failure you’ve developed. The most common treatment options include:
Beta-Blockers
Beta-blockers are a class of drugs that slow your heart rate, lower blood pressure, and reduce the force of contraction in your heart muscle. They work by blocking the effect of certain hormones that cause the heart to beat quickly.
Beta-blockers can help you feel better if you have high blood pressure or chest pain (angina) due to coronary artery disease or atherosclerosis. But they’re not recommended for people who have low blood pressure (hypotension).
ACE Inhibitors
ACE inhibitors are a class of drugs that lower blood pressure and reduce the workload of the heart. They are used to treat high blood pressure, heart failure, and kidney problems.
ACE inhibitors include:
- Captopril
- Enalapril
- Lisinopril
- Ramipril
Digoxin
If you have heart failure, your doctor may prescribe digoxin. This medication is used to slow the heart rate and increase its force of contraction in order to improve blood flow to the body.
Diuretics
Diuretics, such as hydrochlorothiazide (HCTZ), furosemide and torsemide help your kidneys get rid of excess fluid. If you have heart failure or high blood pressure, your doctor may prescribe a diuretic.
Diuretics can cause side effects like dehydration and electrolyte imbalances. They also interact with other medications. Be sure to talk to your doctor about any drug interactions before taking them.
Aldosterone Antagonists
Aldosterone antagonists work by blocking the effect of aldosterone, a hormone that causes your body to hold on to sodium and water. This excess fluid can cause heart failure symptoms, including swelling and shortness of breath.
Aldosterone antagonists are used to treat primary hypertension (high blood pressure) or heart failure. They work best when combined with other medications that block the action of angiotensin II (a hormone secreted by the kidneys).
In Conclusion
Heart failure can be managed with a variety of medications, and in some cases, it may even go away on its own. If you have heart failure, talk to your doctor about what treatments might help you feel better and live longer. We hope this article has given you some insight into the different types of treatments available and how they work!
If you or anyone you know has been experiencing symptoms of heart failure, feel free to reach out to Dr. C Raghu, one of India’s leading cardiologists.
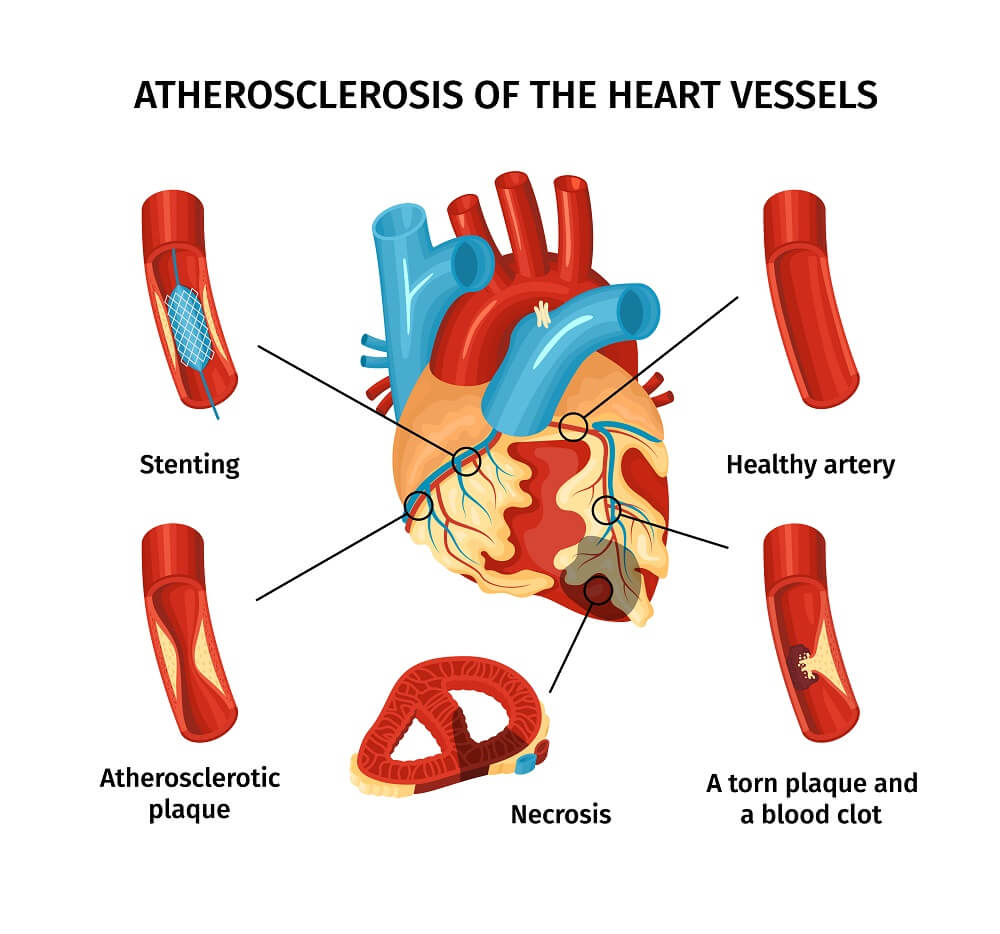
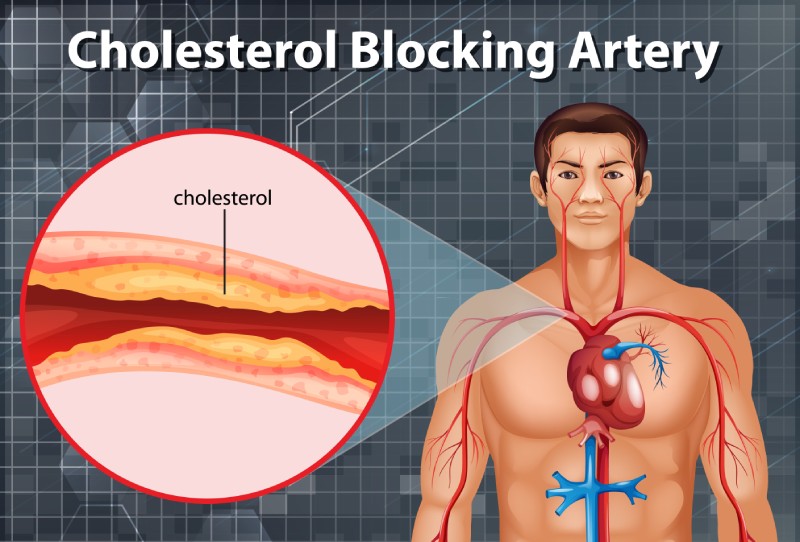
Coronary artery disease (CAD) is the most common type of heart disease, in which the coronary arteries ( blood vessels that supplies oxygen and nutrients to the heart muscle) become rigid and narrowed due to buildup of plaque (deposition of cholesterol) in the inner walls of the heart. This restricts the flow of oxygen rich blood to the heart muscle, which may result in angina (chest pain) and shortness of breath. If the plaque ruptures or due to a complete blockage in the artery, it may result in heart attack or sudden cardiac death.
Causes:
Build of cholesterol plaques within the blood vessels is termed atherosclerosis.
The plaque makes the inner walls of the artery sticky, so that the inflammatory cells, lipoproteins, and calcium travelling through the blood stream and adhere to the plaque. The plaque gradually enlarges, narrowing the blood vessel lumen, restricting blood flow to the heart muscle and thus reducing the supply of oxygen and nutrients to the heart.
Signs and symptoms:
- Angina (chest pain) – on exertion and in severe cases even at rest
- Shortness of breath – on exertion and in severe cases even at rest
- Palpitations (irregular heartbeats or skipped beats)
- Tachycardia (fast heartbeat)
- Weakness or dizziness
- Nausea
- Sweating
- Fatigue, mainly after exercise or any activity
Risk factors:
- Age: Risk for damaged or narrowed arteries increases with age.
- Gender: Men are at greater risk of developing CAD. In women, risk increases after menopause.
- Family history: Risk increases if any family member has coronary artery disease.
- Smoking: People who have the habit of smoking and who are exposed to smoke are at increased risk of CAD.
- High blood pressure: It results in the narrowing and hardening of the walls of arteries.
- High blood cholesterol levels: It can increase the risk of atherosclerosis.
- Diabetes: High degree of association – 2 to 4-fold greater risk
- Obesity: Overweight increases the risk of CAD.
- Life style activities: Reduced physical activity, high stress and unhealthy diet also contribute to the development of CAD
- Mental Stress: Responsible for young heart attacks Other possible risk factors, according to research, include:
- Sleep apnea: It is a condition in which the person may experience intermittent cessation of breathing during sleep, resulting in reduced oxygen levels in the blood. Sleep apnea may cause an increase in the blood pressure and high strain on the heart, leading to CAD.
- Increased C-reactive protein (CRP) levels in blood: CRP levels are increased mostly if there is any inflammation in the body. It is a risk factor for CAD.
- High triglycerides (a type of lipid).
- High homocysteine (amino acid) levels.
- Preeclampsia (high blood pressure during pregnancy).
- Alcohol use can lead to heart muscle damage.
- Autoimmune diseases such as Rheumatoid arthritis and Lupus.
Complications:
If left untreated, CAD can lead to life threatening complications such as:
- Angina: Due to narrowed blood vessels, the heart muscles receive inadequate oxygen laden blood, causing chest pain or shortness of breath.
- Heart attack: The plaque may rupture forming a clot and blocking the blood flow to the heart muscle.
- Heart failure: Due to reduced oxygen and nutrient rich blood flow, the heart is unable to pump enough blood, thus increasing its workload. Over time, it may lead to weakening of heart muscle, also called heart failure.
- Arrhythmia: Reduced amount of blood supply may lead to abnormal heart rhythms
- Sudden cardiac death
Diagnosis:
The diagnostic work up includes a physical examination, in addition to medical history, family history, risk factors and any signs and symptoms of CAD. Further diagnostic tests may be recommended:
- Electrocardiogram (ECG): It records the heart’s electrical activity and helps to determine the blood flow in the heart as well as heart muscle stress.
- Echocardiogram: It uses sound waves to produce clear images of the heart and helps to identify the damaged heart muscles and valves.
- Stress test: The test involves performing any high intensity activity like walking fast on a treadmill or bicycling under medical supervision, and close monitoring of heart function during the physical activity. Symptoms, ECG, blood pressure and heart rhythm are closely monitored during the test. Based on the findings the probability of having significant coronary artery disease would be determined. This test has many limitations and fallacies.
- Cardiac catheterization and angiogram: A special medication called contrast is injected into the coronary blood vessels using a thin, flexible tube called catheter. The catheter is inserted through a small incision at the groin or through the wrist to visualise the blood vessels supplying the heart.
- Heart scan: Computerized tomography (CT) technologies are used to identify the calcium deposits in the blood vessel of the heart, which indicates CAD.
Coronary Artery Disease Treatment:
Lifestyle changes:
- Quit smoking
- Avoid processed foods and eat high protein and fiber rich diet
- Exercise regularly and lose excess weight
- Manage stress
- Control diabetes and blood pressure
Medications:
The doctor may prescribe medications, which help in reducing symptoms and severity of disease such as:
- Dyslipidemic agents such as statins, ezeimibe to lower the blood cholesterol levels
- Aspirin, a blood thinner, to prevent blood clots’ formation that might obstruct the coronary arteries
- Beta blockers decrease the heart rate and blood pressure and reduce the oxygen demands of the heart.
- Calcium channel blockers to lower blood pressure and improve blood supply to the heart.
- Trimetazidine and Ranolazine are anti-anginal drugs to reduce chest pain
- Nitroglycerin to dilate the coronary arteries and reduce chest pain
- Angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs) to decrease blood pressure and improve heart efficiency.
Surgical procedures:
- Angioplasty and stent placement: It is also called as percutaneous coronary revascularization, and involves inserting a thin, flexible tube (catheter) into the narrowed coronary artery, followed by a wire with deflated balloon to the narrowed area. The balloon is inflated to widen the blood vessel; a stent may also be placed to keep the artery patent.
- Coronary artery bypass surgery: A graft is created using any blood vessel in the body, to bypass the blocked coronary arteries.
Prevention:
To maintain healthy arteries and to prevent coronary artery disease, some measures need to be taken such as lifestyle modifications which includes avoiding smoking and alcohol use, exercising regularly to maintain healthy weight, controlling sugar and cholesterol levels in blood and also eating a healthy diet.
Copyright © 2023, Dr. Raghu. All rights reserved.
+91 95424 75650
+91 95424 75650