Hyderabad, July 9 (IANS) Vitamin D deficiency is not a major risk factor for heart attacks or atrial fibrillation. It is a soft target and not a hard point in management of heart disease, opines leading cardiologist Dr C. Raghu. According to him, the major risk factors for heart attacks remain hypertension, diabetes, high cholesterol and family history In an interview with IANS, the senior interventional cardiologist and clinical director at Yashoda Hospitals, Secunderabad, explained some of the recent advances in the domain of heart heath. Q: How do you look at the recent study that Vitamin D might reduce the risk of heart attacks and prevent irregular heartbeats? A: These are not therapies for these problems. These are in addition to what all other measures a person takes. People might think that Vitamin D is the only thing. Heart disease is a multi-factor disorder. Still, the standard risk factors remain diabetes, hypertension, high cholesterol and family. These have strong correlation. Vitamin D to treat or to prevent heart attack is still a long term goal even going by this study. Many studies might come on various factors and they might choose positive benefits but for these positive benefits to translate to clinical medicine is a long process. There are many medications which can definitely reduce the heart event rate but for this many factors have to be addressed properly. Vitamin D is a very soft target not a hard point. It is not the only thing. People should not think that if I take Vitamin D, I will be okay. I think fundamentals remain the same. Diabetes, hypertension, high cholesterol and physical activity continue to remain major pillars. These risk factors have to be addressed to prevent heart attack. Q: How common is atrial fibrillation in the Indian context? A: Atrial fibrillation is worsening like heart disease. It is a multifactorial disease. Most of the patients of atrial fibrillation are elderly women they have underlying hypertension, diabetes and they have stiff heart syndrome. In this group of patients prone to develop atrial fibrillation there are many hard end points which we can address rather than focusing on Vitamin D. Vitamin D is not a major risk factor. In the Indian context also, atrial fibrillation is an emerging epidemic. The main reasons are still uncontrolled high blood pressure, aging process and stiff heart. These will continue to be the main promoters of development atrial fibrillation. As a doctor, I would prefer to treat them rather than treat a very soft end point like Vitamin D. Q: Will the use of higher doses of Vitamin D for a longer period negatively impact patients? If yes, what are the risks? A: Yes. That is one of the major reasons why one should be very careful. Somebody might think what is the harm in consuming Vitamin D as it is a simple medication but that’s not the way. Unsupervised Vitamin D use for a prolonged period of time can lead to lot of medical complications. Some people might develop renal dysfunction, some people might develop hyperparathyroidism or produce more calcium (hypercalcemia). There are a lot of metabolic problems that may happen if somebody takes long duration vitamin D without proper medical supervision. Presence of deficiency of Vitamin D and its correction are not the same. Sometimes correction of vitamin D deficiency might not reduce the primary problem. Prolonged consumption of Vitamin D and unsupervised especially elderly people tend to develop more complications. One should be cautious in taking Vitamin D without supervision. Having said that, there are a lot of natural sources for production of Vitamin D. I would prefer my patients to have a natural way to produce Vitamin D by their body as a medication. I encourage my patients to have 15 minutes of sunlight at least 2-3 times a week and at least once a week, do traditional remedies like application of castor oil to promote internal development of Vitamin D. These are simple measures one can take and naturally produce Vitamin much more quantitatively better. Q-What are the other new or recent discoveries for managing heart health? A: In the management of heart health, what the recent advances suggest is to stick to the traditional risk factors only. We now have a lot of objective data. Let us consider Lipid. We have a lot of data which emerged in the last one decade indicating that people should target their Lipid. There is a lot of misinformation and misconception which are being propelled by various sources indicating that one should not believe in Lipid but we have strong data on the management of Lipid. We have clear-cut numbers. What is LDL cholesterol a person should have. The numbers are different for a person who does not have heart attack and the one who had heart attack. For a person who does not have a heart attack but has only Diabetes, we aim for LDL of less than 70. Same for a person with heart attack we aim for LDL cholesterol of less than 55. Same for a person who has got a high risk we aim for less than 35. Previously we never used to aim for such low levels of LDL cholesterol. Now we understand that a very low level of LDL cholesterol will reduce the risk of having a cardiac event. This is one of the important advances which I think people have to be aware of. There are different cut-off levels. When people go to a laboratory, the normal value of cholesterol creates confusion. They will try to remain at a much higher level than what is desired for them. A lot of personalised medicine is coming for different subsections of people. It might look very less interesting for people but it is a very important and also inexpensive way to reduce the risk of heart attack. One of the common ways to reduce heart attacks is to use aspirin. We all think that taking aspirin a day reduces the risk. Now with the availability of new data, we can understand that certain groups of patients get benefited and certain groups of patients can get harmed. What we understand is that aspirin used for patients less than 60 who have diabetes and hypertension, they get better whereas for patients who are more than 60 years, we have to select patients who are going to be benefited rather than using aspirin for all of them as a blanket. Aspirin therapy is very useful for prevention of heart stroke in people who already had a heart attack but for those people who never had a heart attack in the past or who never had bypass surgery, it is better to limit the use of aspirin among people who are less than 60. So we have to differentiate between those who had heart attack angioplasty vis-a-vis those who never had an event and use aspirin selectively for people who already had heart attack and for those who did not have heart attack, we need to calculate the risk and then only use benefit of the therapy. We now understand that women tend to have a higher risk of heart attack than what we were thinking in the past. Now a days, we see a lot of women also developing heart attacks. That is due to multiple to new risk factors which we were hitherto not knowing. These risk are enhancers: for women who tend to premature menopause naturally or surgically, they will have a higher risk of heart attack. Premature means less than 40. Women who have immunological disorders like Rheumatoid arthritis or SLE tend to have higher chances of heart attack. Such women possibly take aspirin to prevent heart attack. In addition to traditional risk factors, we have risk enhancing factors for women and people who have South Asian ancestry like Indians. They play an important role for the development of heart attacks. South Asian ancestry people tend to have higher risk of heart attack especially those with a family history of heart attacks in less than 50 years of age. Those people are at higher risk of developing heart attacks. That is also considered a risk enhancer. That’s why you see a lot of young people developing heart attacks among the Indian population because of our propensity. It is not considered as risk factor but considered risk enhancer Compared to the past we are seeing more and more women developing heart attacks at younger age. Previously we were not seeing this. Women who tend to have higher blood pressure during pregnancy may develop heart attacks. This is also considered a risk enhancer for a heart attack. Q: Is building more data helping understand the risk factors and risk enhances better? A: We continue to get data. The larger the data set, better we can understand the association. Risk scores have also been developed. These risk scores help us to estimate what is the risk of a particular person to a heart attack in the next 10 years. With these risk scores, objective risk assessment is possible compared to what we used to assess risk in a subjective way. For the Indian population who are having a risk of more than 10 per cent, it is considered high risk in India. This means more than 10 per cent chance of having a heart attack in the next 10 years is considered high risk in India. Indian race and south Asian ancestry itself is a risk enhancer. If risk calculation is more than 10 per cent, it is considered high risk whereas the same for any other race, we consider high risk if it is more than 20 per cent. The bar is set at the lower level for the Indian population. Clinical practitioners and even lay persons calculate risk score. Easiest risk score they use is by the American Heart Association. This risk score calculator is developed in the form of an app and available on Google as well as Apple store. It is an ASCVD risk calculator. This is an objective app. A person can calculate the risk. Risk score gives an idea what medication one should take. For example whether a person should take aspirin, cholesterol lowering medication, blood pressure medication, and what lifestyle modification is required. One can also know how much risk reduction is possible by adhering to those lifestyle modifications. Indians calculating risk on ASCVD need to choose an ‘other’ group which happens to be of South Asian ancestry. More than 20 per cent risk score is considered high risk in the American context while for Indian people, more than 10 per cent risk is considered high risk.

Book Online Consultaion
What Are the 5 Most Common Heart Problems?
Subscribe the Hearty Life Blogs

DR. RAGHU | Best Cardiologist in Hyderabad
Cardiology Coronary, Vascular and
Structural Interventions
cardiologist / Dr Raghu
A healthy heart is essential for overall well-being, and summer presents an opportunity to embrace these seasonal delights. So, make the most of the bountiful produce available, experiment with new recipes, and prioritize your heart health this summer.
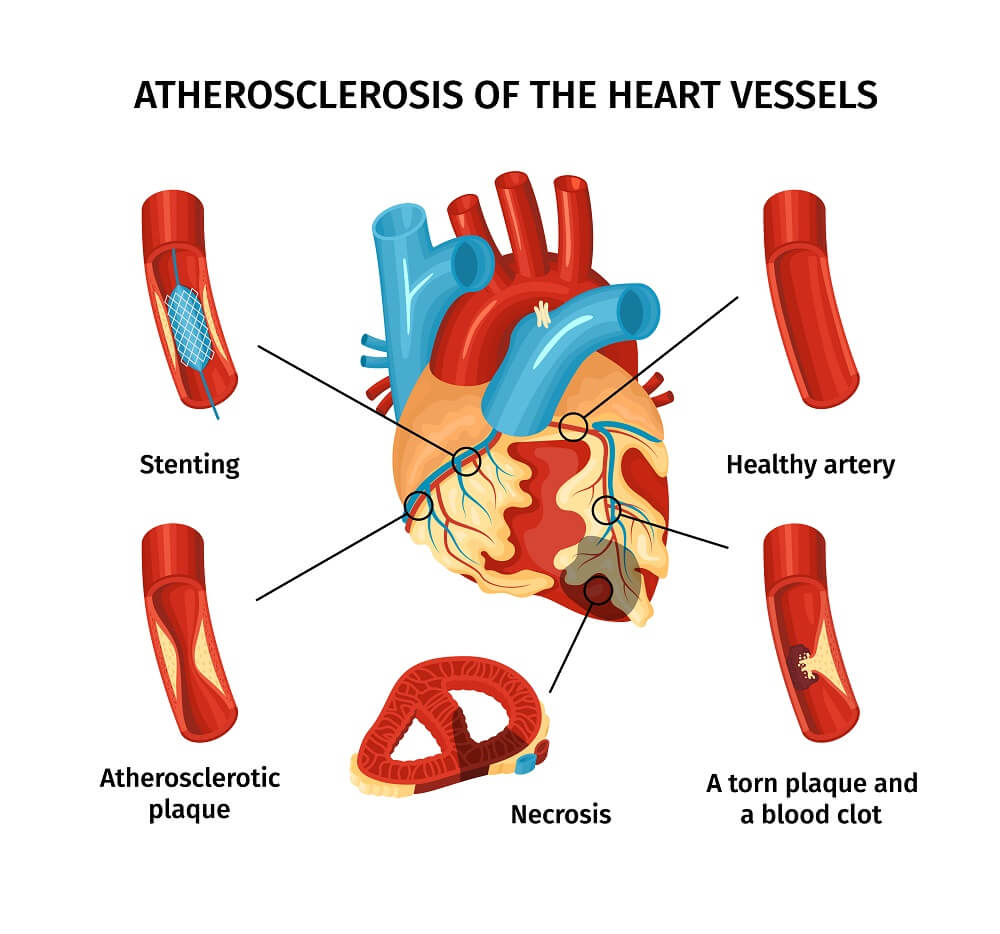
A heart attack is a life-threatening condition that requires emergency medical interventions, such as angioplasty in the heart.
A heart attack, medically known as a myocardial infarction, is a severe medical emergency that can cause lasting damage to the heart muscle and even lead to death. As a leading cause of death worldwide, it shouldn't be taken lightly.
A heart attack, medically known as a myocardial infarction, is a severe medical emergency that can cause lasting damage to the heart muscle and even lead to death. As a leading cause of death worldwide, it shouldn't be taken lightly.
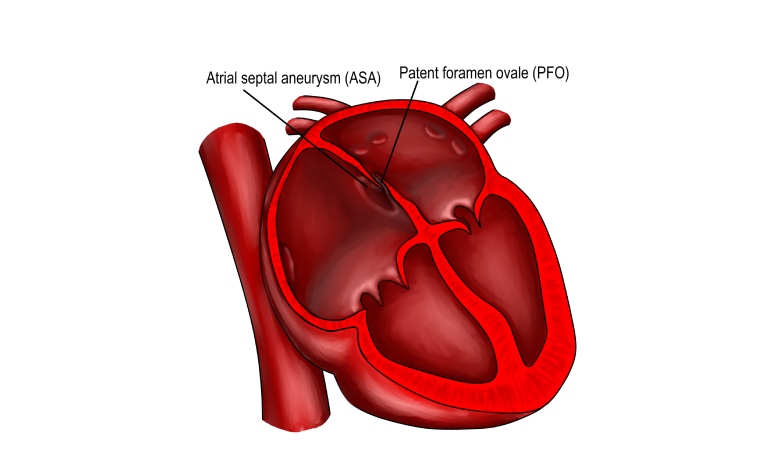
The heart is a vital organ that supplies blood to the muscles and tissues and keeps your body running. In our previous articles, we’ve discussed common conditions that affect the heart, such as congestive heart failure and atrial fibrillation. Take a look at our blog for more information. While much is discussed about these common ailments, other conditions like patent foramen ovale (or PFO) can also affect the heart. So, what exactly is PFO? And how does it affect your cardiac health? In this article, we’ll explore the ins and outs of this lesser-known condition. Patent Foramen Ovale (PFO) is a hole in the heart that can be congenital or acquired. The foramen ovale is a flap-like opening between the heart’s upper chambers. It usually closes within three to six months after birth and becomes a part of your heart’s septum. But if that doesn’t happen, you may have a PFO. In most cases, a PFO is present at birth (congenital). However, one can also develop it as an adult due to injury, infection, or inflammation of the tissue around the heart (acquired). If you’ve been diagnosed with a patent foramen ovale, you’re likely wondering if it poses a threat to your cardiac health. Fortunately, this condition is usually asymptomatic and does not require treatment. However, it can be a risk factor for stroke and heart attack in some people. PFO can also be the underlying cause of other conditions, such as: That makes it crucial to stay in touch with your doctor and monitor your heart health to keep these conditions at bay. If you’re lucky, a PFO will cause no noticeable symptoms. However, if it results in a drop in your blood oxygen levels, you may experience a variety of symptoms, including: Treatment options for a PFO include: If you experience symptoms, your doctor may recommend lifestyle changes or medication as treatment options. Now you know what a patent foramen ovale is and why it’s so important to get checked out if you have symptoms. If you are diagnosed with a PFO, your doctor may recommend treatment based on your symptoms and medical history. That said, PFO does not always require treatment. Some people have been living with it for years without any issues at all. Dr. C Raghu is an eminent cardiologist who specializes in interventional cardiology. If you or anyone you know has been diagnosed with a patent foramen ovale, feel free to consult Dr. Raghu to explore your treatment options.
What is Patent Foramen Ovale?
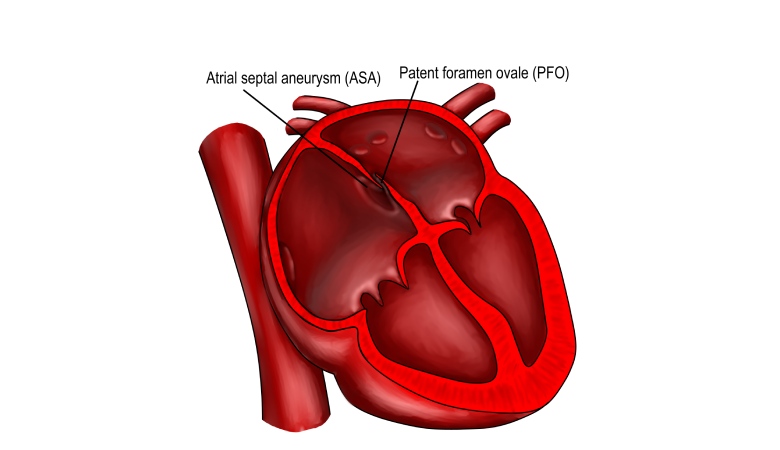
Should You Be Worried About Patent Foramen Ovale?
Signs and Symptoms of PFO
What Are the Treatment Options for Patent Foramen Ovale?
In Conclusion

Dr. RAGHU
Cardiology Coronary, Vascular and
Structural InterventionsConditions & Diseases

Angioplasty

Aortic Stenosis

Atrial Fibrillation

Atrial Septal Defect
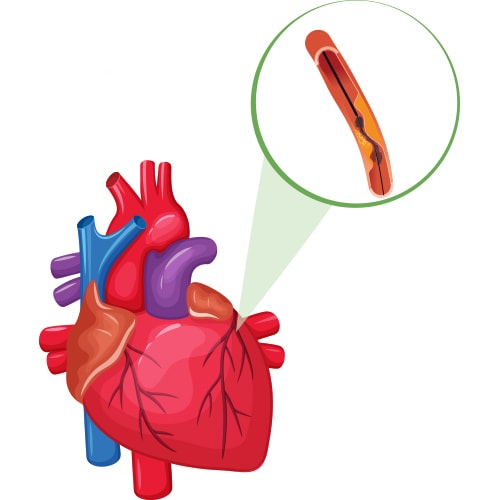
What Is Coronary Angiography?
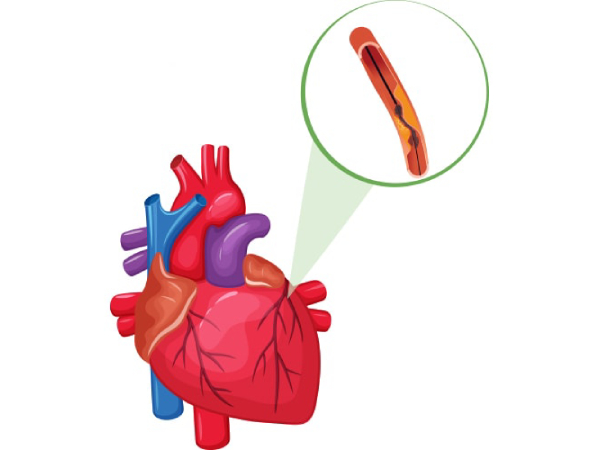
Coronary angiography is a procedure that uses X-rays to visualize and inspect arteries. It shows if there are any blocked arteries and how well your heart muscle is working.
During this procedure, a catheter is inserted into an artery in your arm or groin and advanced into one of your coronary arteries. Thereafter, contrast dye is injected into the coronary artery to make it visible on X-ray images.

The procedure can help identify blockages in the heart’s blood vessels and guide treatment decisions for patients at risk of developing heart disease or having a heart attack due to narrowed or blocked blood vessels that supply oxygenated blood to various organs.
When Is Coronary Angiography Performed?
Coronary angiography is typically performed if you have chest pain or other symptoms that suggest the presence of heart disease. If you have had a heart attack or have been diagnosed with coronary artery disease. It can be used in conjunction with an exercise stress test.
How Is Coronary Angiography Done?
If you’re scheduled for coronary angiography, here’s what you can expect:
- The doctor will give you a sedative, usually in the form of an injection, at the start of your procedure.
- They’ll insert a catheter into one of your arteries, either in your groin or wrist, and guide it through your blood vessels to reach your heart.
- They’ll inject a special dye (contrast agent) into the coronary arteries that supply blood to your heart muscle so that they can see them clearly on X-rays taken after injecting this contrast agent.
Where Is Coronary Angiography Performed?
Coronary angiography is performed in a cath lab (catheterization laboratory). The cath lab is a room with special equipment for performing coronary angiography and other procedures that entail inserting a long, thin tube (called a catheter) into the blood vessels of your heart.
Why Is Coronary Angiography So Common Nowadays?
Advancements in medical science have made coronary angiography more accessible to patients. The procedure has become simple and the risk has reduced significantly. Also, unhealthy diets and lifestyle choices put more people at risk of developing cardiac ailments. That’s why coronary angiography is commonly performed now-a-days.
What are the risks involved in Coronary angiography?
In expert hands coronary angiography is a near-zero risk procedure. The risk of complications can be broadly categorized into:
Less severe complications
- bleeding under the skin at the wound site (haematoma) – this should improve after a few days, but contact your Cardiologist if you’re concerned. Application of ice packs would be helpful.
- bruising – it’s common to have a bruise in your groin or arm for a few weeks. Application of ice packs would be helpful.
- allergy to the contrast dye used, causing symptoms such as a rash and a headache – this is uncommon, but you should discuss any allergies with your cardiologist before having the procedure
Severe complications
The chance for developing a serious complication during coronary angiogram is 1 in 1000. People with serious underlying heart problems are most at risk. Discuss with your cardiologist about the risks before the procedure.
- damage to the artery in the arm or groin in which the catheter was inserted, with the blood supply to the limb possibly being affected
- heart attack – a serious medical emergency where the heart’s blood supply is suddenly blocked
- stroke – a serious medical condition that occurs when the blood supply to the brain is interrupted
- damage to the kidneys caused by the contrast dye
- tissue damage caused by X-ray radiation if the procedure is prolonged
- death
In Conclusion
Coronary angiography is used to diagnose and treat heart diseases, before cardiac surgery, angioplasty-stent procedures as well as other conditions such as aneurysms in blood vessels. It helps doctors identify underlying causes of heart failure and determine the proper course of treatment.
Dr. C Raghu is a renowned cardiologist with decades of experience in interventional cardiology. He is one of the pioneers of trans-radial procedures in India. Consult him if someone is in need for coronary angiogram.
Coronary angiography is a common diagnostic test used by doctors to identify conditions, such as coronary artery disease and aneurysms. In our previous blog, we discussed how the procedure is carried out and when it’s used. Click here to check it out.
Angiography is a minimally invasive procedure, which makes it extremely safe. However, it can involve a few minor side effects. The benefits outweigh the risks for most patients. However, in some cases, coronary angiography can result in serious complications.
In this article, we’ll delve deeper into the risks and side effects associated with coronary angiography.
Common Side Effects of Coronary Angiography
If you’re planning to visit the doctor for an angiography, you can expect one or more of the following side effects:
- Bruising
- Swelling
- A buildup of blood (resulting in a bump)
All these symptoms are localized to the area where the cut was made for inserting the catheter. Most patients experience a gradual improvement in these side effects without medical intervention. You can take painkillers to relieve discomfort after the procedure.
Complications of Coronary Angiography
If you’re lucky, you’ll come out of coronary angiography with minor bruising and swelling. However, some patients develop the following complications:
- An infection near the cut :- It makes the area around the cut red, swollen, and tender.
- An allergic reaction to the dye :- It usually results in an itchy rash.
In both cases, proper use of medications can help control the side effects. For instance, antibiotics can be used in the case of an infection. Similarly, your doctor might prescribe antihistamines if you experience an allergic reaction.
It’s worth mentioning that coronary angiography comes with a few potential serious complications. These include:
- Kidney damage (from the dye)
- Cardiac arrest or stroke
- Internal bleeding (due to damaged blood vessels)
- Anaphylaxis (due to severe allergic response to the dye)
The good news is that these complications are extremely rare (affecting less than one in every 1000 patients). Also, kidney damage due to angiography is usually temporary. Moreover, internal bleeding can be contained with the help of catheter based approaches.
Seeking Medical Help
Complications from coronary angiography are rare. Nevertheless, it’s a good idea to consult your doctor if you notice anything unusual after the procedure. For instance, if the leg or arm where the cut was made looks pale or feels numb, it’s a cause for concern. Similarly, if you notice bleeding, redness, or a firm lump near the cut, it could indicate a potential infection. It’s always a good idea to watch out for these signs and consult your doctor for timely treatment.
In Conclusion
Coronary angiography is a safe and minimally invasive procedure. It can cause minor side effects, such as pain and swelling. However, in extreme cases, it can also lead to a heart attack or kidney damage. It’s crucial to talk to your doctor about the potential risks before going in for the procedure.
Dr. C Raghu has more than two decades of experience in treating patients with different heart conditions. If you have queries or concerns about coronary angiography, feel free to reach out to Dr. Raghu today.
Book Online Consultaion
What Are the Risks of Coronary Angiography? – Blog
Subscribe the Hearty Life Blogs
In our previous articles, we’ve discussed the symptoms of heart failure and the steps to diagnose the same. However, the course of treatment varies for every patient based on the type of heart failure they’ve developed.
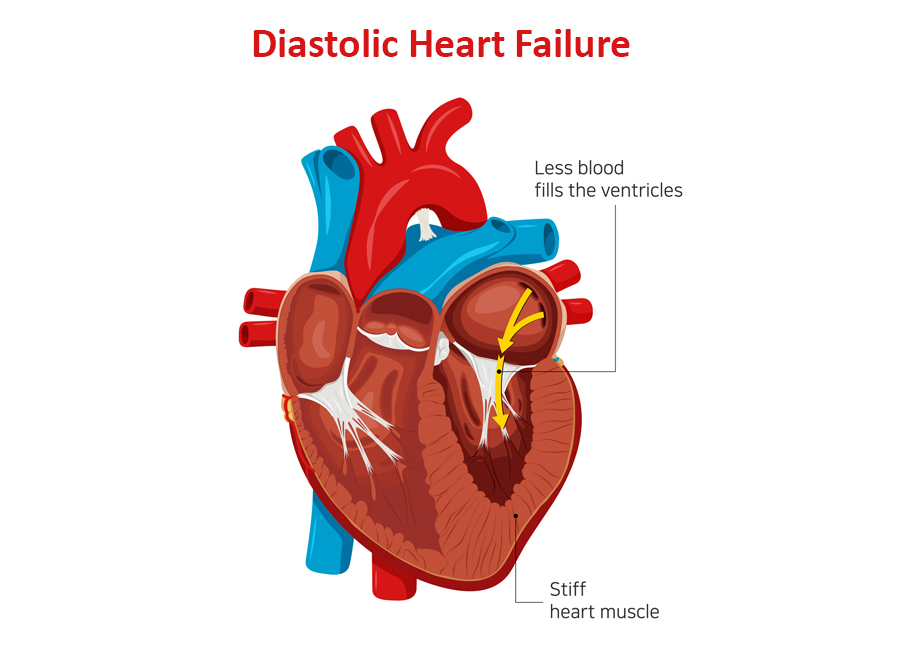
Depending on the part of the heart’s pumping cycle that’s been affected, there are two types of heart failure. In this blog, we’ll take a closer look at diastolic dysfunction and its symptoms.
What Causes Diastolic Dysfunction?
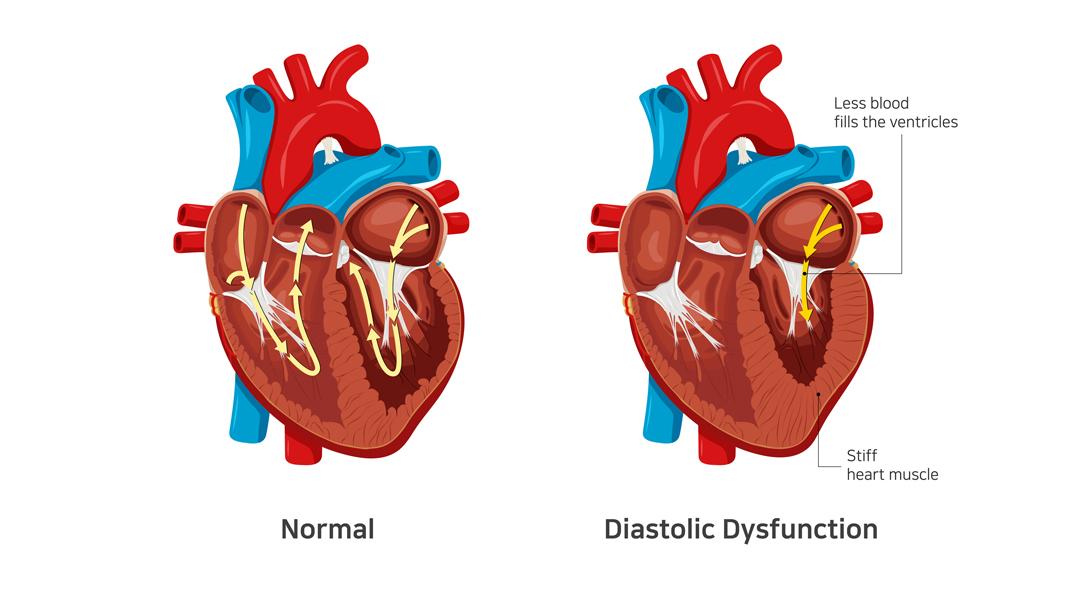
The diastolic phase refers to the part of the heart’s pumping cycle when the ventricles (lower chambers) relax and let blood flow in from the atria (upper chambers). Diastolic dysfunction is a condition in which the ventricles don’t relax enough. That, in turn, prevents the normal amount of blood from entering the heart.
Diastolic dysfunction is caused when the heart muscles become thicker and stiffer than usual. It’s more common in older women with hypertension and diabetes. If left untreated, it can lead to diastolic heart failure (also known as heart failure with preserved ejection fraction).
Related : Understanding Congestive Heart Failure Symptoms
What Does Preserved Ejection Fraction Mean?
Ejection fraction refers to the volume of blood pumped out from the heart’s left ventricle with each contraction. For a healthy heart, the number falls in the range of 55% to 65%. A lower ejection fraction is one of the most common indicators of heart failure.
However, it’s worth noting that many people with diastolic dysfunction have an ejection fraction of 50% or more (which is known as preserved ejection fraction). That means the left ventricle expels an adequate amount of oxygenated blood.
However, the heart muscle doesn’t relax enough to let a sufficient quantity of blood in. That, in turn, causes the excess blood to back up in the lungs and results in fluid buildup in the feet and abdomen.
How to differentiate systolic from diastolic dysfunction ?
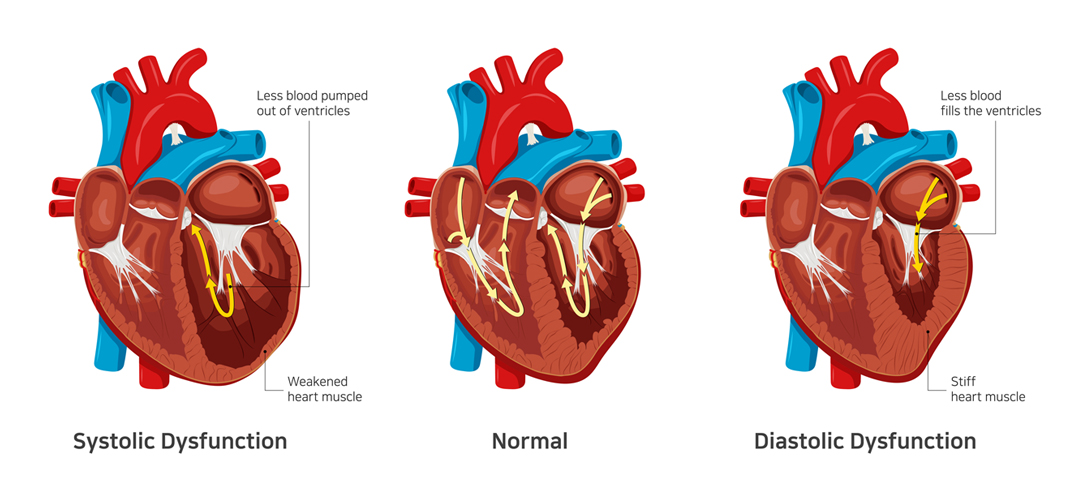
In contrast to systolic dysfunction where the heart muscle is “weak”, in diastolic dysfunction the heart is “stiff”. This means that the heart is unable to pump blood out of the heart in systolic dysfunction whereas the heart is unable to accept further blood in diastolic dysfunction. Both conditions lead to congestion or fluid accumulation in various organs of the body. Differentiation of heart failure from systolic and diastolic dysfunction is not possible as both diseases present with similar symptoms.
Which conditions lead to Diastolic dysfunction?
- Diastolic dysfunction appears consequent to uncontrolled or long-standing diabetes
- Hypertension
- Obesity as well as elderly people
- Women and atrial fibrillation
The best way to prevent and treat diastolic dysfunction is by effective control of the diseases mentioned above.
Symptoms of Diastolic Dysfunction
The most common symptom of diastolic dysfunction is congestion and shortness of breath due to the buildup of blood and fluid in the lungs. Breathing difficulties can get particularly worse during exertion or when lying.
Other symptoms of diastolic dysfunction include:
- Coughing and wheezing (due to lung congestion)
- Loss of appetite and nausea (due to fluid buildup around the liver and in the stomach)
- Swollen feet, legs, and abdomen (due to fluid accumulation)
If you experience any of the given symptoms, it’s crucial to consult a doctor for a proper diagnosis.
Treatment of Diastolic Dysfunction
Treatment of diastolic dysfunction involves a combination of medications (diuretics or water pills) and lifestyle changes. In severe cases, a patient might need left ventricular assist devices or a heart transplant.
Is Diastolic Dysfunction Serious?
In the long run, diastolic dysfunction can lead to diastolic heart failure. That, in turn, increases your risk of hospitalization and death. Therefore, you should pay close attention to your symptoms and reach out to a doctor whenever you notice anything unusual.
Dr. C Raghu is a renowned cardiologist who specializes in interventional cardiology. He has decades of experience in treating patients with different heart conditions. If you or anyone you know has developed symptoms like shortness of breath, swollen feet, loss of appetite, etc., contact Dr. Raghu to explore your treatment options.
Book Online Consultaion
What Are the Symptoms of Diastolic Dysfunction ? – Blog
Subscribe the Hearty Life Blogs
Congestive heart disease or heart failure is a serious condition that can be life-threatening (if left untreated). It can diminish blood supply to vital organs, such as the brain, liver, and kidneys. That, in turn, can lead to organ damage.

In this blog, we’ll delve deeper into the causes and types of congestive heart failure. Also, we’ll understand the outlook for patients living with the condition. Let’s get started.
What Are the Causes of Congestive Heart Failure?
Congestive heart failure is characterized by a gradual deterioration in the heart’s ability to pump blood throughout the body. It can result in various symptoms, such as swelling in the abdomen, feet, and legs, shortness of breath, fatigue, weight gain, and loss of appetite. Read our blog post on heart failure symptoms for more details.
Typically, the condition is the result of an abnormality in the cardiac muscles that interferes with the heart’s pumping function. It can be due to a congenital defect or an underlying illness that exerts the heart muscles.
The most common causes of congestive heart disease include :
- Hypertension
- Diabetes
- Coronary artery diseases
- Damaged or dying heart tissue due to a previous heart attack
- Cardiomyopathy
- Heart rhythm disturbances
- Heart valve damage
The following factors also increase an individual’s risk of developing the condition:
- A family history of cardiovascular diseases
- Tobacco smoking
- Alcohol consumption
- Sedentary lifestyle
- Substance abuse
Types of Congestive Heart Failure
Depending on the part of the heart’s pumping cycle that’s been affected, congestive heart failure can be of two types: systolic heart failure and diastolic heart failure.
In systolic heart failure, the left ventricle becomes thin and weak and is unable to push an adequate amount of oxygen-rich blood into the arteries. It’s also known as heart failure with reduced ejection fraction.
In diastolic heart failure, the ventricles become thick and stick, due to which the heart can relax and let an adequate amount of blood fill the chambers. It’s also known as heart failure with preserved ejection fraction.
Congestive heart failure can also be categorized into two types depending on the side of the heart that’s affected. This includes left-sided heart failure and right-sided heart failure.
Acute Congestive Heart Failure
The American College of Cardiology and the American Heart Association have outlined four distinct stages of the progression of heart failure. Stage four, or the most advanced stage, is characterized by acute heart failure.
At this stage, a patient experiences severe symptoms that don’t respond to standard treatments. They might need frequent hospitalization or specialized treatment to stay out of the hospital.
Congestive Heart Failure Prognosis
There’s no known cure for congestive heart failure. However, timely diagnosis, proper treatment, and lifestyle changes can be instrumental in improving a patient’s quality of life and longevity. Doctors usually use a cardiopulmonary stress test to predict your prognosis.
The prognosis of congestive heart failure for a patient depends on various factors, including their age, sex, medical history, and lifestyle. Chronic ailments like diabetes can worsen your prognosis. Also, the stage at which heart failure is diagnosed influences the outlook.
Dr. C Raghu is a world-renowned cardiologist who’s helped thousands of patients with cardiac ailments. He specializes in interventional cardiology and has nearly two decades of experience. If you or anyone you know has been diagnosed with congestive heart disease, feel free to consult Dr. Raghu right away.
Book Online Consultaion
Congestive Heart Disease: An Overview – Blog
Subscribe the Hearty Life Blogs
Copyright © 2023, Dr. Raghu. All rights reserved.
+91 95424 75650
+91 95424 75650