In our previous blogs, we’ve discussed various tests doctors use to monitor cardiac health and diagnose conditions like coronary artery disease and heart failure.
It’s worth noting that commonly used diagnostic tests like coronary angiography rely on a procedure called cardiac catheterization. In this blog, we’ll discuss the procedures in greater detail to help you understand the benefits and risks.
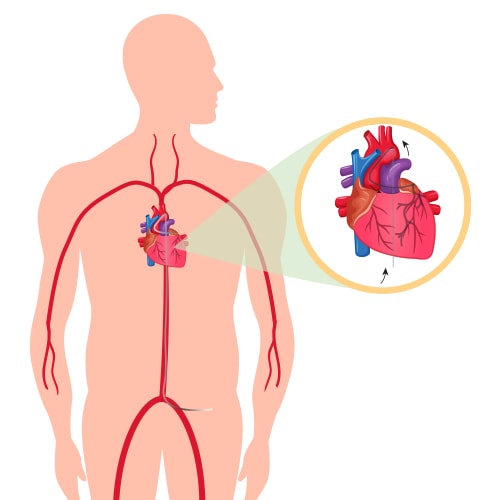
Cardiac catheterization is a procedure in which doctors insert a thin, flexible tube called a catheter into your heart through an artery.
What Is Cardiac Catheterization?
Cardiac catheterization is a procedure that uses a thin tube (called a catheter) to examine the heart and blood vessels. The catheter is inserted into a blood vessel in the groin or arm. Thereafter, it’s advanced through the blood vessels and into the heart to measure pressures within different chambers of your heart.
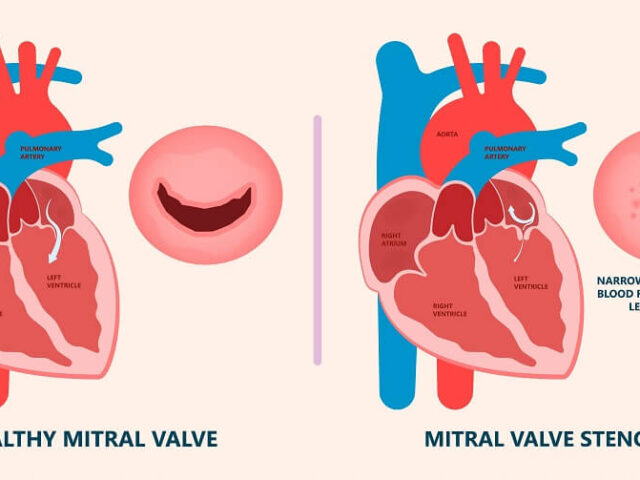
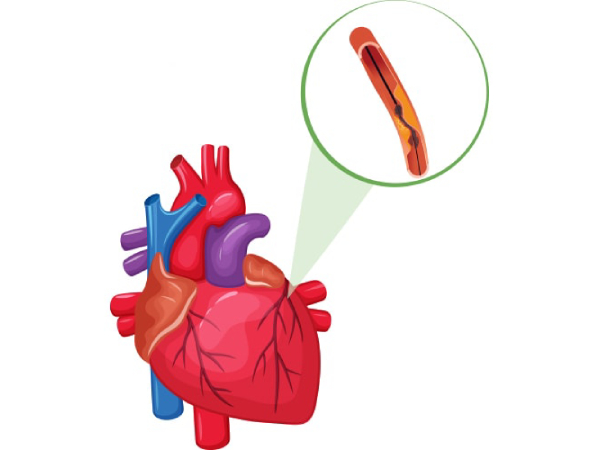
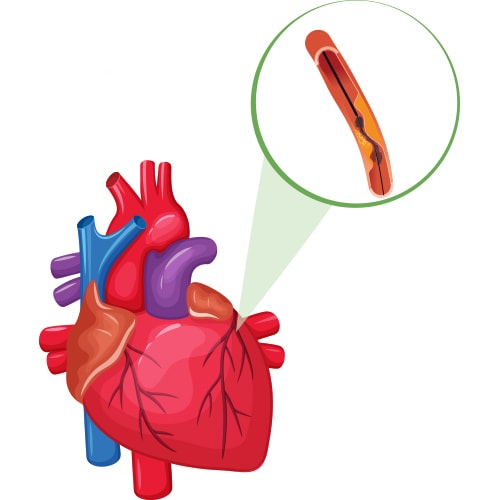
The test lets doctors see if there’s any blockage in the blood vessels that supply blood to your heart. Also, they can assess whether the cardiac muscles and valves are in proper working condition. Also, it may be used to insert wires (called stents) in coronary arteries if they become narrow due to plaque buildup or after an injury.
To perform balloon angioplasty, the doctor inflates a tiny balloon at one end of the catheter inside one of the blocked coronary arteries. It creates more space for oxygen-rich blood flow through your coronary arteries and helps improve symptoms like chest pain caused by a heart attack.
How Does Cardiac Catheterization Work?
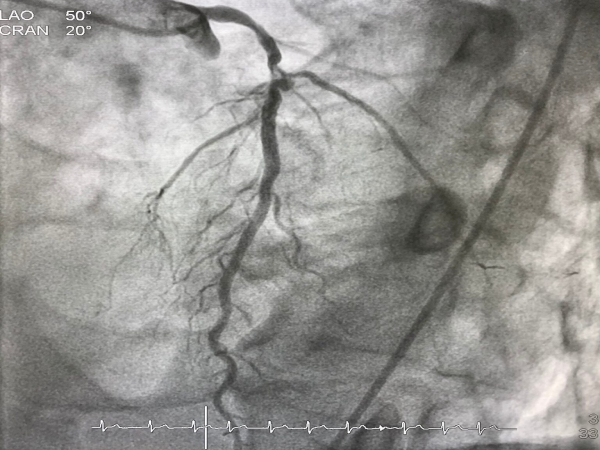
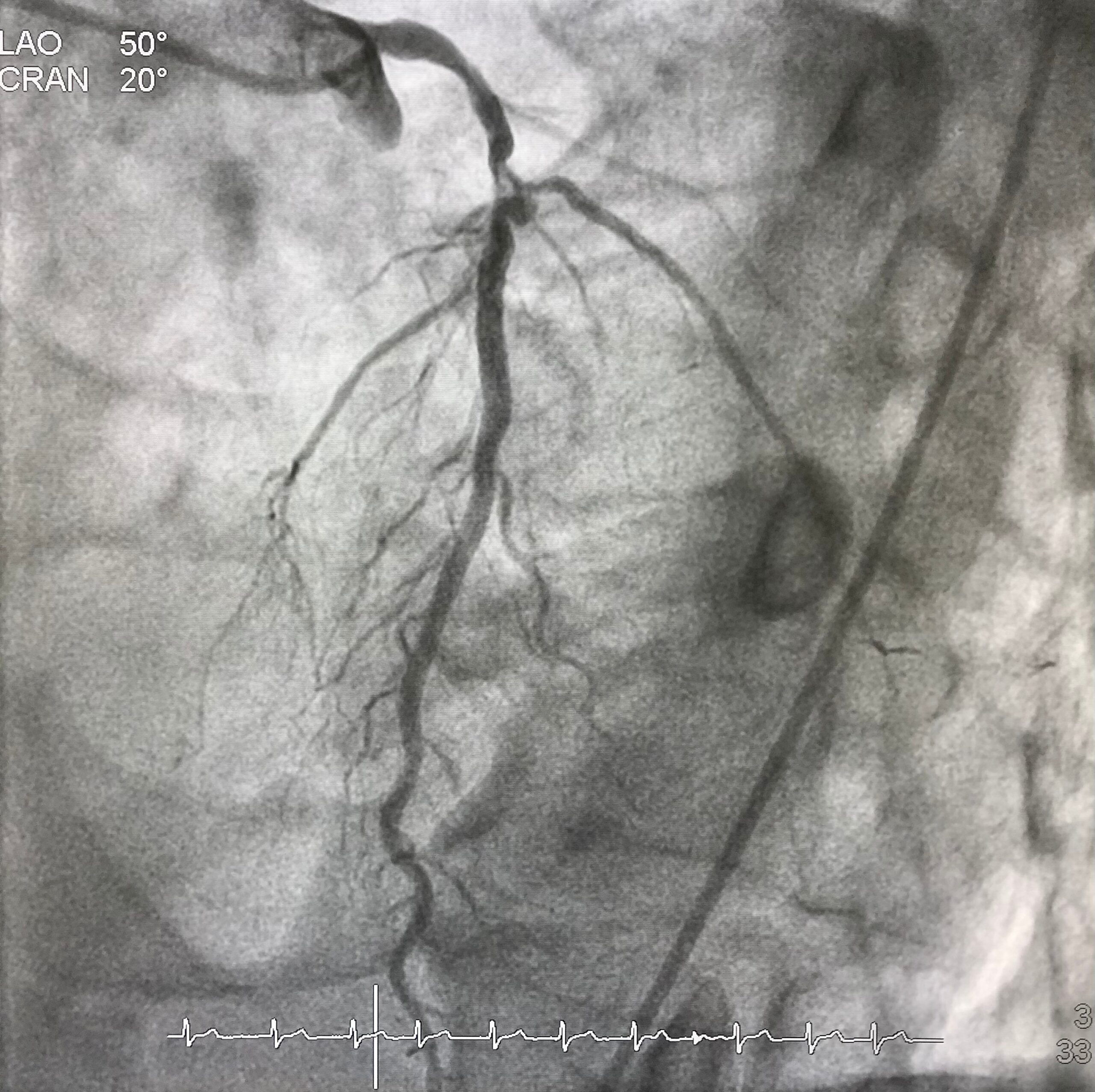
In this procedure, a doctor inserts the catheter into a blood vessel in your arm or groin. The catheter is guided through the blood vessels to the heart, where it’s used to look for blockages or other problems in the coronary arteries that supply oxygen-rich blood to your heart muscle.
Afterward, a dye is injected into your bloodstream from an intravenous (IV) line connected to your vein. It helps doctors see how well blood flows through different parts of your heart on X-rays taken during the procedure.
Why Do Doctors Use Cardiac Catheterization?
Cardiac catheterization can be used to diagnose or treat various heart ailments. It can help your doctor determine if your heart is getting enough blood and if there are any blockages in the arteries that supply blood to the rest of your body. Also, it can help identify any problems with the heart muscles and valves.
What Are the Risks of Cardiac Catheterization?
While the risk of complications from cardiac catheterization is low, there are some things you should know before your procedure. For example, you might also experience bleeding or bruising around where the cut was made.
The most severe risk is having a stroke due to excess pressure in the brain caused by increased blood flow due to plaque shaving off from arteries. Other risks include allergic reactions to dyes, bleeding at the puncture site where the catheter was inserted, and infection.
Conclusion
Cardiac catheterization is a standard procedure that can be done in a cath lab or hospital. It allows doctors to check for problems with your heart and blood vessels. Ask your doctor any questions about how long it will take and whether there are any risks associated with cardiac catheterization before scheduling an appointment for this test.
Dr. C Raghu is an accomplished cardiologist with decades of experience in interventional cardiology. If you or anyone you know is experiencing symptoms of cardiac ailments, book an appointment with Dr. Raghu today.