What Is Coronary Angiography?
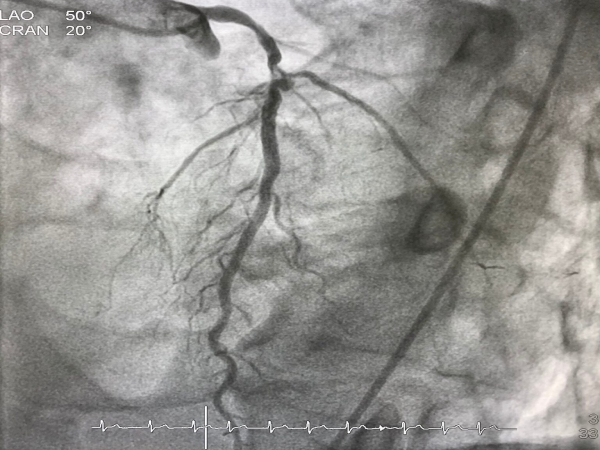
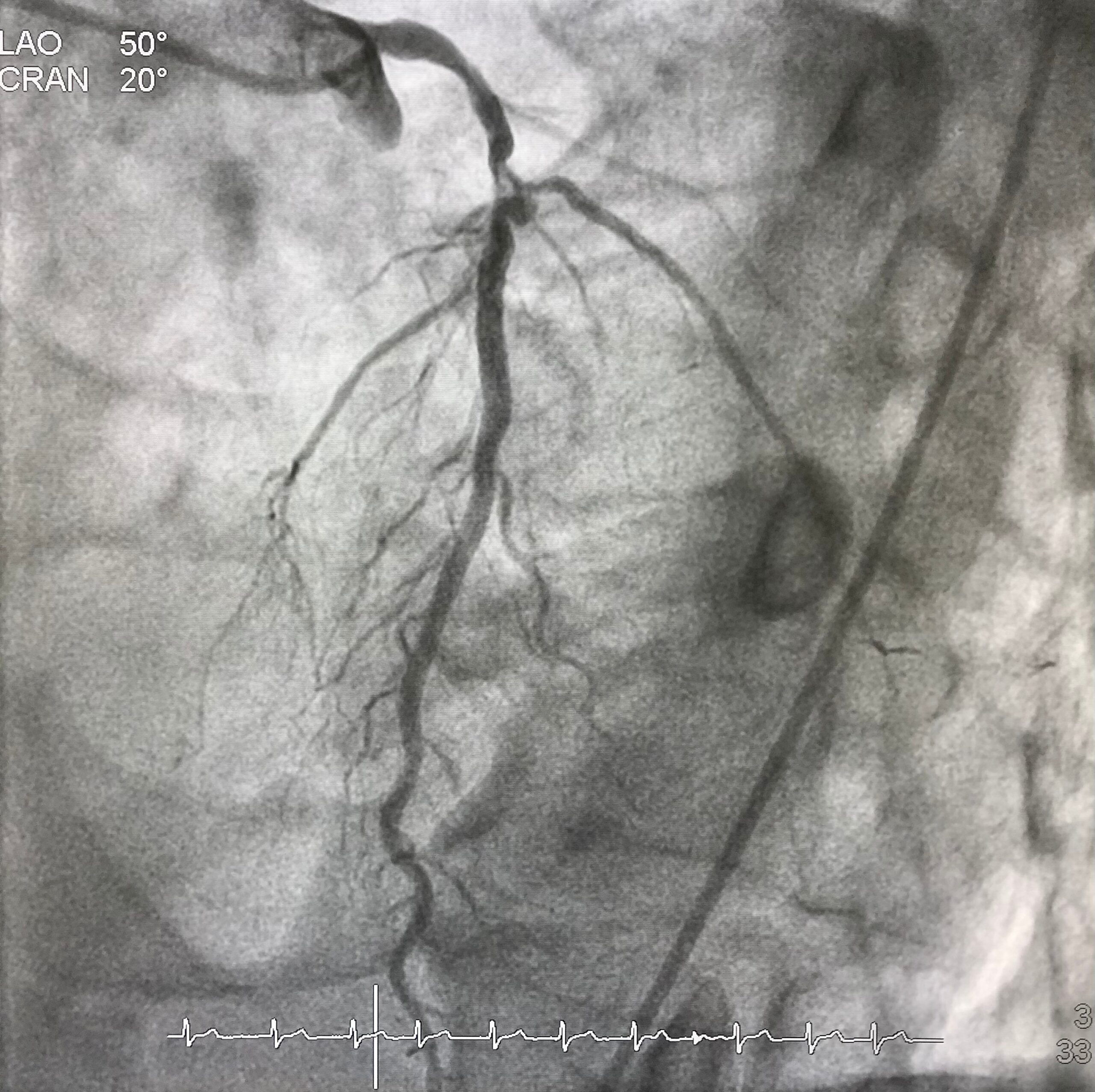
Coronary angiography is a procedure that uses X-rays to visualize and inspect arteries. It shows if there are any blocked arteries and how well your heart muscle is working.
During this procedure, a catheter is inserted into an artery in your arm or groin and advanced into one of your coronary arteries. Thereafter, contrast dye is injected into the coronary artery to make it visible on X-ray images.

The procedure can help identify blockages in the heart’s blood vessels and guide treatment decisions for patients at risk of developing heart disease or having a heart attack due to narrowed or blocked blood vessels that supply oxygenated blood to various organs.
When Is Coronary Angiography Performed?
Coronary angiography is typically performed if you have chest pain or other symptoms that suggest the presence of heart disease. If you have had a heart attack or have been diagnosed with coronary artery disease. It can be used in conjunction with an exercise stress test.
How Is Coronary Angiography Done?
If you’re scheduled for coronary angiography, here’s what you can expect:
- The doctor will give you a sedative, usually in the form of an injection, at the start of your procedure.
- They’ll insert a catheter into one of your arteries, either in your groin or wrist, and guide it through your blood vessels to reach your heart.
- They’ll inject a special dye (contrast agent) into the coronary arteries that supply blood to your heart muscle so that they can see them clearly on X-rays taken after injecting this contrast agent.
Where Is Coronary Angiography Performed?
Coronary angiography is performed in a cath lab (catheterization laboratory). The cath lab is a room with special equipment for performing coronary angiography and other procedures that entail inserting a long, thin tube (called a catheter) into the blood vessels of your heart.
Why Is Coronary Angiography So Common Nowadays?
Advancements in medical science have made coronary angiography more accessible to patients. The procedure has become simple and the risk has reduced significantly. Also, unhealthy diets and lifestyle choices put more people at risk of developing cardiac ailments. That’s why coronary angiography is commonly performed now-a-days.
What are the risks involved in Coronary angiography?
In expert hands coronary angiography is a near-zero risk procedure. The risk of complications can be broadly categorized into:
Less severe complications
- bleeding under the skin at the wound site (haematoma) – this should improve after a few days, but contact your Cardiologist if you’re concerned. Application of ice packs would be helpful.
- bruising – it’s common to have a bruise in your groin or arm for a few weeks. Application of ice packs would be helpful.
- allergy to the contrast dye used, causing symptoms such as a rash and a headache – this is uncommon, but you should discuss any allergies with your cardiologist before having the procedure
Severe complications
The chance for developing a serious complication during coronary angiogram is 1 in 1000. People with serious underlying heart problems are most at risk. Discuss with your cardiologist about the risks before the procedure.
- damage to the artery in the arm or groin in which the catheter was inserted, with the blood supply to the limb possibly being affected
- heart attack – a serious medical emergency where the heart’s blood supply is suddenly blocked
- stroke – a serious medical condition that occurs when the blood supply to the brain is interrupted
- damage to the kidneys caused by the contrast dye
- tissue damage caused by X-ray radiation if the procedure is prolonged
- death
In Conclusion
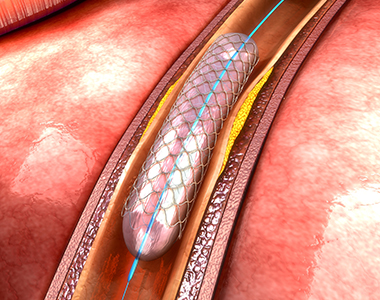
Coronary angiography is used to diagnose and treat heart diseases, before cardiac surgery, angioplasty-stent procedures as well as other conditions such as aneurysms in blood vessels. It helps doctors identify underlying causes of heart failure and determine the proper course of treatment.
Dr. C Raghu is a renowned cardiologist with decades of experience in interventional cardiology. He is one of the pioneers of trans-radial procedures in India. Consult him if someone is in need for coronary angiogram.