A weak heart, also known as heart failure, is a condition characterized by the heart's inability to pump blood efficiently, leading to reduced circulation and inadequate oxygen supply to the body's tissues.
Heart Failure / Dr Raghu
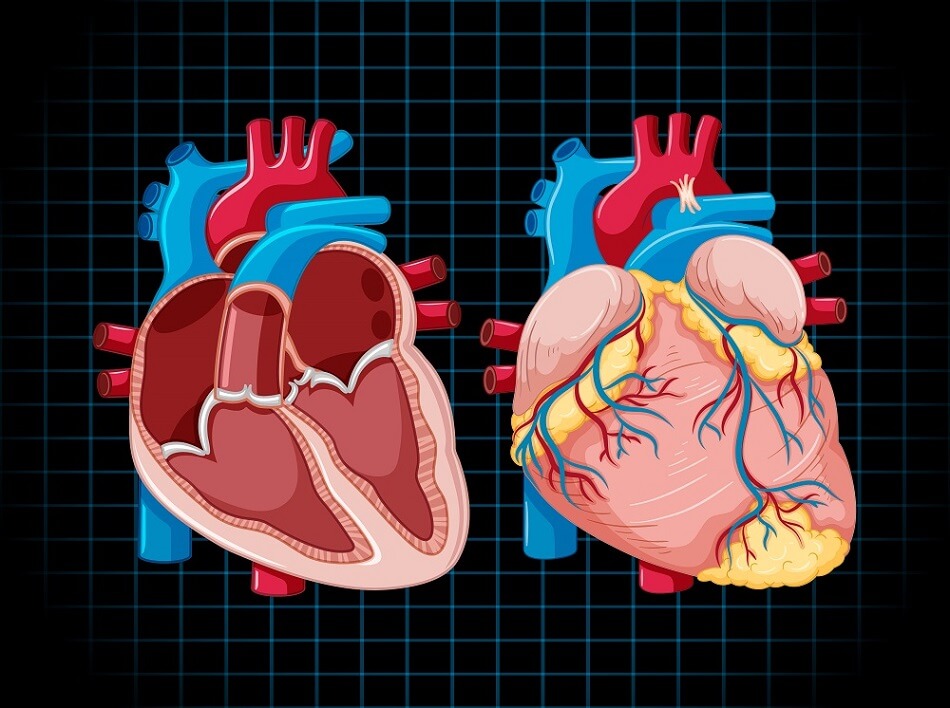
The heart is a vital organ that supplies blood to muscles and organs throughout the body. It delivers oxygen and nutrients to the cells and removes waste products. Heart problems can occur when the heart does not function properly.
A heart attack is a life-threatening condition that requires emergency medical interventions, such as angioplasty in the heart.
Recent studies have shown that irregular sleep may also increase the risk of cardiovascular problems. In severe cases, it can result in complications, such as heart attacks.
Heart disease is a leading cause of death worldwide. Various factors, such as stress, underlying medical conditions, and a sedentary lifestyle, make an individual more vulnerable to heart disease.
Heart failure is a condition in which the heart can’t pump enough blood to meet the body’s needs. It’s a serious condition that requires treatment by your doctor, but there are several options available. If you’re concerned about heart failure and want to know more about your options for treatment, keep reading.

What Is Heart Failure?
Heart failure occurs when your heart doesn’t pump blood as well as it should due to one or more problems with its cardiac function. The heart can’t pump blood as well because it has to work harder than normal just in order to keep up with the body’s needs for oxygen and nutrients. The extra effort causes structural changes in the heart over time.
Types of Heart Failure
Although there are many specific types of heart failure, the two broad categories are as follows:
- Heart failure with preserved ejection fraction or diastolic heart failure
- Heart failure with reduced ejection fraction or systolic heart failure
Heart failure can also be categorized depending on the side of the heart that’s affected. These include:
- Left-sided heart failure
- Right-sided heart failure
The treatment of heart failure depends on the type of heart failure you’ve developed. The most common treatment options include:
Beta-Blockers
Beta-blockers are a class of drugs that slow your heart rate, lower blood pressure, and reduce the force of contraction in your heart muscle. They work by blocking the effect of certain hormones that cause the heart to beat quickly.
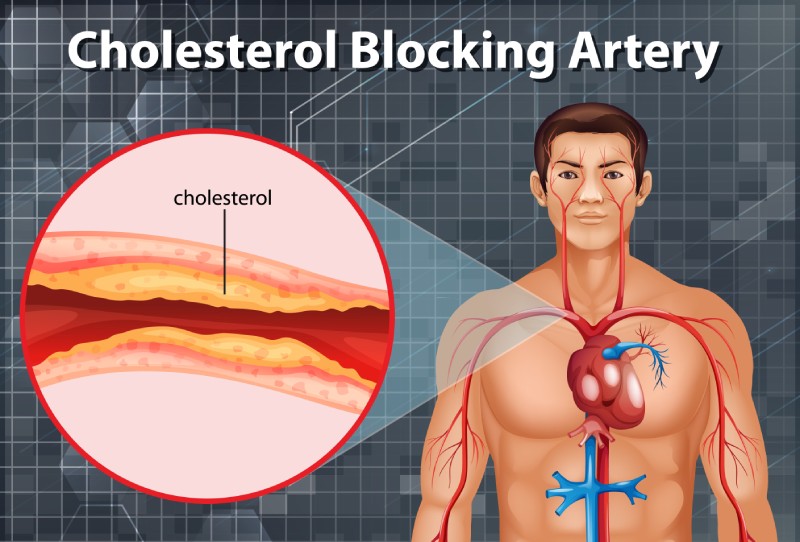
Beta-blockers can help you feel better if you have high blood pressure or chest pain (angina) due to coronary artery disease or atherosclerosis. But they’re not recommended for people who have low blood pressure (hypotension).
ACE Inhibitors
ACE inhibitors are a class of drugs that lower blood pressure and reduce the workload of the heart. They are used to treat high blood pressure, heart failure, and kidney problems.
ACE inhibitors include:
- Captopril
- Enalapril
- Lisinopril
- Ramipril
Digoxin
If you have heart failure, your doctor may prescribe digoxin. This medication is used to slow the heart rate and increase its force of contraction in order to improve blood flow to the body.
Diuretics
Diuretics, such as hydrochlorothiazide (HCTZ), furosemide and torsemide help your kidneys get rid of excess fluid. If you have heart failure or high blood pressure, your doctor may prescribe a diuretic.
Diuretics can cause side effects like dehydration and electrolyte imbalances. They also interact with other medications. Be sure to talk to your doctor about any drug interactions before taking them.
Aldosterone Antagonists
Aldosterone antagonists work by blocking the effect of aldosterone, a hormone that causes your body to hold on to sodium and water. This excess fluid can cause heart failure symptoms, including swelling and shortness of breath.
Aldosterone antagonists are used to treat primary hypertension (high blood pressure) or heart failure. They work best when combined with other medications that block the action of angiotensin II (a hormone secreted by the kidneys).
In Conclusion
Heart failure can be managed with a variety of medications, and in some cases, it may even go away on its own. If you have heart failure, talk to your doctor about what treatments might help you feel better and live longer. We hope this article has given you some insight into the different types of treatments available and how they work!
If you or anyone you know has been experiencing symptoms of heart failure, feel free to reach out to Dr. C Raghu, one of India’s leading cardiologists.
In our previous blogs, we’ve explored the causes, symptoms, and treatment options of heart failure. Also, we’ve outlined different types of heart failure in detail. You can click here to check out our previous blogs.
In this article, we’ll discuss left ventricular ejection fraction, one of the most common parameters doctors use to diagnose heart failure. Let’s dive right in.

What Is Ejection Fraction?
Simply put, ejection fraction is a measure of the amount of blood pumped out from the heart’s lower chambers (ventricles). Ejection fraction can be of two types:
- Left ventricular ejection fraction
- Right ventricular ejection fraction
Right ventricular ejection fraction is the percentage of deoxygenated blood the right ventricle pushes into the lungs. On the other hand, left ventricular ejection fraction (LVEF) is the percentage of oxygen-rich blood pumped out from the left ventricle into the arteries that carry blood to vital organs, muscles, and tissues.
Typically, doctors use the term “ejection fraction” when they refer to LVEF. If your heart is healthy and well functioning, the ejection fraction will range between 55% to 66%. An ejection fraction lower than 50% is a sign of systolic heart failure (or heart failure with reduced ejection fraction).
However, it’s possible for you to develop heart failure with an ejection fraction above 50%. In such cases, there’s a problem with the relaxed (or diastolic) phase of the heart’s pumping cycle. The condition is known as diastolic heart failure (or heart failure with preserved ejection fraction).
It’s worth noting that an abnormally high ejection fraction (above 70%) could be an indication of a heart condition like hypertrophic cardiomyopathy.
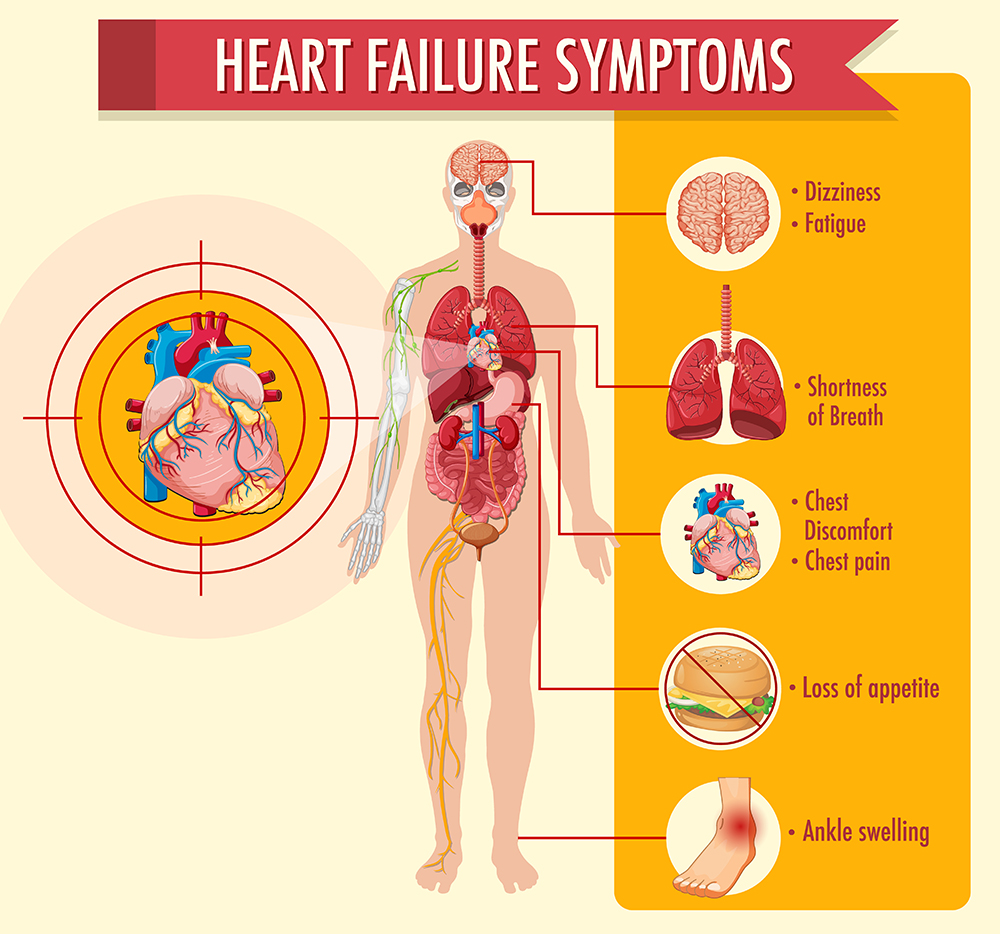
Symptoms of Low Ejection Fraction
As mentioned earlier, a low ejection fraction (below 50%) is a sign of heart failure. It means that the heart is unable to pump an adequate amount of blood into the arteries. It results in a shortage of blood supply to various organs. Also, it causes excess blood to back up in the lungs.
The most common symptoms of low LVEF include:
- Shortness of breath
- Mental confusion
- Pale or bluish skin color
- Swelling in the abdomen, feet, and legs
- Weight gain (due to fluid buildup)
- Loss of appetite
- Coughing and wheezing
Treatment of Low Ejection Fraction
Cardiologists use a wide array of tests to detect a low ejection fraction and its underlying cause. These include ECG, echocardiogram, chest X-ray, etc. The course of treatment depends on the underlying disorder that’s causing low LVEF.
The most common treatment options include medications, such as digoxin (to strengthen the heart’s contractions), beta-blockers (to ease the heart’s workload), and diuretics (to minimize fluid buildup in the body).
Additionally, your doctor will recommend lifestyle changes, such as weight loss, exercise, and a healthy diet to improve LVEF. Also, it’s a good idea to avoid alcohol consumption and tobacco smoking.
In Conclusion
A low LVEF is a prominent sign of systolic heart failure. It can cause symptoms like shortness of breath and fluid buildup in the body. If you’ve been diagnosed with a low ejection fraction, consult your doctor to explore your treatment options.
Dr. C Raghu is an eminent cardiologist with years of experience. He specializes in interventional cardiology. If you or anyone you know is experiencing symptoms of heart failure, feel free to consult Dr. Raghu today.
Book Online Consultaion
Left Ventricular Ejection Fraction Blog
Subscribe the Hearty Life Blogs
Heart failure is an umbrella term for a set of physical symptoms arising due to the gradual deterioration in the heart’s pumping ability. The term “congestive heart failure” was traditionally used because the condition resulted in fluid buildup and congestion in the lungs. However, doctors and medical researchers have found that it causes a wide array of other symptoms. That’s why they now refer to the condition as heart failure. A healthy human heart relaxes and contracts nearly 100,000 times a day and pumps more than 2,000 gallons of blood throughout the body. The cardiovascular system also includes a network of arteries and veins to transport deoxygenated and oxygenated blood to and from the heart. If any part of the system falters, it can disrupt the flow of blood to vital organs. Heart failure is characterized by a progressive decline in the heart’s power to pump blood. When that happens, the heart goes through a series of structural changes (knowns as cardiac remodeling) and beats faster to pump more blood. Also, the blood vessels constrict to stabilize blood pressure and restrict blood supply to non-critical organs like the skin and kidneys. When blood flow to the kidneys reduces, it compels the body to retain more fluid and sodium. All these short-term fixes result in more damage and cause even more stress to the heart muscles. That, in turn, results in further deterioration of the heart’s pumping action. The heart failure symptoms vary depending on whether they’re caused due to a lack of oxygen or an increase in fluid build. Lack of oxygen supply results in the following heart failure symptoms : Excess sodium and fluid buildup in the body causes the following heart failure symptoms: The most common causes of heart failure include: There are various ways to categorize congestive heart failure. Depending on the part of the heart’s pumping that’s affected due to heart failure, it can be of the following types: Also, depending on the side of the heart that’s affected, heart failure can be categorized as left-sided failure and right-sided failure. The treatment approach a doctor will use depends on the type of heart failure a patient has developed. The American College of Cardiology and the American Heart Association has outlined four stages to denote the progression of heart failure. While Stage A is characterized by risk factors like underlying medical conditions, stage B shows structural changes in a patient’s heart. The more advanced stages (C and D) present visible symptoms. Heart failure (also known as congestive heart failure) is a progressive condition caused by the heart’s inability to pump blood adequately. It results in symptoms like shortness of breath, fatigue, weight gain, and brain fog. Dr. C Raghu is an eminent cardiologist with more than two decades of experience. If you or someone you know has developed congestive heart failure symptoms, consult Dr. Raghu to explore your treatment options.
What Happens in Congestive Heart Failure?
Congestive Heart Failure Symptoms: A Closer Look

Causes and Types of Congestive Heart Failure
Stages of Heart Failure
In Conclusion
Book Online Consultaion
Understanding Congestive Heart Failure Symptoms Blog
Subscribe the Hearty Life Blogs

DR. RAGHU
Cardiology Coronary, Vascular and
Structural InterventionsConditions & Diseases

Angioplasty

Aortic Stenosis

Atrial Fibrillation

Atrial Septal Defect
Congestive heart disease or heart failure is a serious condition that can be life-threatening (if left untreated). It can diminish blood supply to vital organs, such as the brain, liver, and kidneys. That, in turn, can lead to organ damage.

In this blog, we’ll delve deeper into the causes and types of congestive heart failure. Also, we’ll understand the outlook for patients living with the condition. Let’s get started.
What Are the Causes of Congestive Heart Failure?
Congestive heart failure is characterized by a gradual deterioration in the heart’s ability to pump blood throughout the body. It can result in various symptoms, such as swelling in the abdomen, feet, and legs, shortness of breath, fatigue, weight gain, and loss of appetite. Read our blog post on heart failure symptoms for more details.
Typically, the condition is the result of an abnormality in the cardiac muscles that interferes with the heart’s pumping function. It can be due to a congenital defect or an underlying illness that exerts the heart muscles.
The most common causes of congestive heart disease include :
- Hypertension
- Diabetes
- Coronary artery diseases
- Damaged or dying heart tissue due to a previous heart attack
- Cardiomyopathy
- Heart rhythm disturbances
- Heart valve damage
The following factors also increase an individual’s risk of developing the condition:
- A family history of cardiovascular diseases
- Tobacco smoking
- Alcohol consumption
- Sedentary lifestyle
- Substance abuse
Types of Congestive Heart Failure
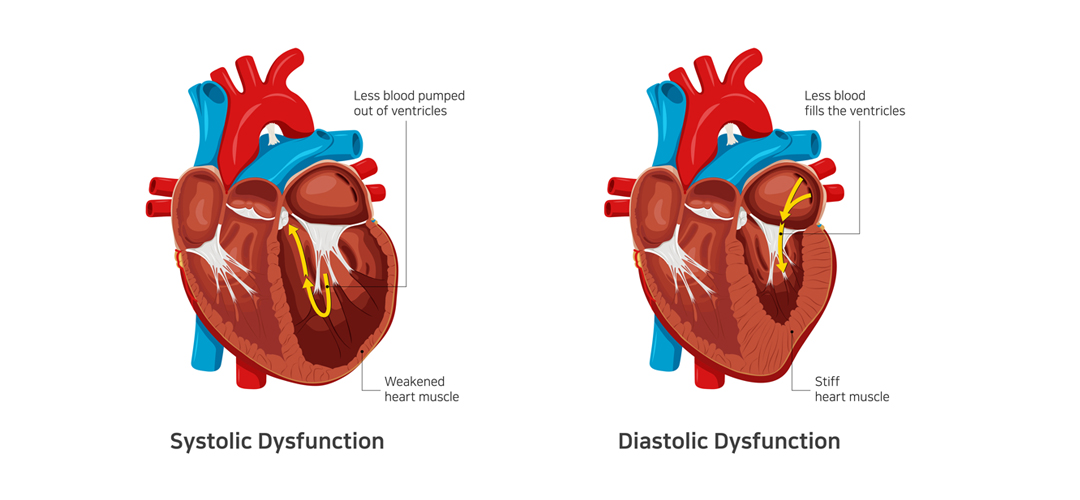
Depending on the part of the heart’s pumping cycle that’s been affected, congestive heart failure can be of two types: systolic heart failure and diastolic heart failure.
In systolic heart failure, the left ventricle becomes thin and weak and is unable to push an adequate amount of oxygen-rich blood into the arteries. It’s also known as heart failure with reduced ejection fraction.
In diastolic heart failure, the ventricles become thick and stick, due to which the heart can relax and let an adequate amount of blood fill the chambers. It’s also known as heart failure with preserved ejection fraction.
Congestive heart failure can also be categorized into two types depending on the side of the heart that’s affected. This includes left-sided heart failure and right-sided heart failure.
Acute Congestive Heart Failure
The American College of Cardiology and the American Heart Association have outlined four distinct stages of the progression of heart failure. Stage four, or the most advanced stage, is characterized by acute heart failure.
At this stage, a patient experiences severe symptoms that don’t respond to standard treatments. They might need frequent hospitalization or specialized treatment to stay out of the hospital.
Congestive Heart Failure Prognosis
There’s no known cure for congestive heart failure. However, timely diagnosis, proper treatment, and lifestyle changes can be instrumental in improving a patient’s quality of life and longevity. Doctors usually use a cardiopulmonary stress test to predict your prognosis.
The prognosis of congestive heart failure for a patient depends on various factors, including their age, sex, medical history, and lifestyle. Chronic ailments like diabetes can worsen your prognosis. Also, the stage at which heart failure is diagnosed influences the outlook.
Dr. C Raghu is a world-renowned cardiologist who’s helped thousands of patients with cardiac ailments. He specializes in interventional cardiology and has nearly two decades of experience. If you or anyone you know has been diagnosed with congestive heart disease, feel free to consult Dr. Raghu right away.
Book Online Consultaion
Congestive Heart Disease: An Overview – Blog
Subscribe the Hearty Life Blogs
Heart failure is a serious condition that can result in organ damage and death (if left untreated). If you want more information about the different types and symptoms of heart failure, take a look at our previous blog posts.
In this article, we’ll explore the different causes of heart failure in greater detail. Let’s get started.
Heart Failure: A Closer Look
Heart failure refers to a condition where the heart is unable to pump blood throughout the body with maximum efficiency. It’s usually the result of progressive weakening, thickening, or stiffening of the heart muscles.
In the past, doctors used to refer to the condition as congestive cardiac failure because it leads to fluid buildup and congestion in the lungs. However, recent research shows that heart failure can cause several other symptoms.
Symptoms of Heart Failure
It’s possible for patients to develop heart failure without showing symptoms for months. That’s because they might attribute signs like confusion and fatigue to other factors, such as old age and stress.
However, if you’re at risk of developing heart failure, you should watch out for the following symptoms:
- Swelling in the abdomen, feet, and legs
- Shortness of breath that worsens due to physical exertion or when lying down
- Weight gain due to fluid buildup
- Loss of appetite
- Pale or bluish skin
Related : Understanding Congestive Heart Failure Symptoms
Causes of Heart Failure
Heart failure can be the result of various underlying conditions, including hypertension, diabetes, chronic respiratory disease, cardiomyopathy, and coronary artery disease. Also, it can be caused by damage to the heart muscles due to a viral or bacterial infection or a previous heart attack.
Moreover, faulty heart valves can strain the cardiac muscles and lead to heart failure. Similarly, heart rhythm disturbances can create structural changes in the left ventricle and cause heart failure.
It’s worth noting that people with a family history of cardiac ailments are more prone to developing heart failure. Also, the risk is higher in seniors and people with an African-American ethnic background. Alcohol consumption, tobacco smoking, and substance abuse also increase the risk.
Types of Heart Failure
Depending on the phase of the heart’s pumping cycle that’s affected by congestive cardiac failure, the condition can be of two types:
- Systolic heart failure – Heart failure due to a problem in the contraction (systolic) phase of the pumping cycle; also known as heart failure with reduced ejection fraction.
- Diastolic heart failure – Heart failure due to a problem in the relaxed (diastolic) phase of the pumping cycle; also known as heart failure with preserved ejection fraction.
Heart failure can also be categorized as:
- Left-sided heart failure (caused by a weak left ventricle)
- Right-sided heart failure (caused by a weak right ventricle)
Related : Types of Heart Failure
Stages of Heart Failure
The American Heart Association (AHA) and the American College of Cardiology (ACC) have identified four distinct stages of heart failure based on the degree of severity. The course of treatment for a patient depends on the stage of heart failure they’re at.
Diagnosing Heart Failure
Heart failure is diagnosed through a series of lab tests, including ECG, echocardiogram, coronary angiography, chest X-ray, brain natriuretic peptide test, etc. Doctors recommend the right combination of tests to identify the causes of heart failure and devise a suitable treatment plan.
Dr. C Raghu is an eminent cardiologist with more than two decades of experience. He specializes in interventional cardiology and has helped a plethora of patients with different heart conditions. If you’ve been diagnosed with heart failure, feel free to consult Dr. Raghu to explore your treatment options.
Copyright © 2023, Dr. Raghu. All rights reserved.
+91 95424 75650
+91 95424 75650